2 Minute Medicine Rewind August 29, 2022
1. In this prospective cohort study, a fatty liver index (FLI) of > 60, suggestive of non-alcohol related fatty liver disease (NAFLD), is positively associated with incidence of irritable bowel syndrome (IBS).
2. Positive association of NAFLD with IBS was only seen in female participants, and not male participants.
Evidence Rating Level: 2 (Good)
Irritable bowel syndrome (IBS) is a very common disorder affecting approximately 4 – 10% of the population characterized by recurrent abdominal pain and altered bowel habits and bloating. The pathophysiology is unclear, but it is thought to be a disorder of gut-brain interaction. The burden of IBS on the healthcare system is quite extensive, and it is important to identify possible contributing factors for prevention. Non-alcohol-related fatty liver disease (NAFLD) is characterized by hepatic steatosis without another clear cause of liver disease and affects approximately 25% of the adult population. There are previous studies that suggest a possible link between the pathogenesis of NAFLD and IBS, including shared pro-inflammatory cytokines and communication between liver-brain-gut neural arc and gut-liver axis. Both NAFLD and IBS have increased in incidence recently, and this study investigates the association of degree of NAFLD, and NAFLD itself with the risk of IBS incidence. There were over 500,000 participants from a large-scale prospective cohort in the United Kingdom from 22 assessment centers across England, Wales, and Scotland enrolled from 2006 to 2010. Participants who were free of IBS with an available fatty liver index (FLI), which is based on body mass index, waist circumference, triglycerides, and gamma-glutamyltransferase (GGT). FLI > 60 was used as an indicator of NAFLD, and patients were classified according to quartile distribution, with the lowest quartile group as a reference group and others as an exposure. The primary endpoint was incident IBS which was determined via ICD-10 codes, and incidence rate was calculated as number of events per 1000 person-years. In total, 7,129 cases of IBS were identified, with a cumulative incidence rate of 1.49%-and 12-year cumulative incidence of 1.8%. Overall, fatty liver was associated with a 21% increased risk of developing IBS (P<.001). In addition, compared with the lowest quartile group, the second and third quartiles were associated with a significantly higher risk of developing IBS. Between patients with NAFLD and without NAFLD according to the FLI, patients with NAFLD showed a 13% higher risk of developing IBS. There were also significant interactions across gender and age, and the positive association was observed in females but not males. A major limitation of this study was that NAFLD presence was based on biochemical and physical parameters, but not in imaging, which is the gold standard for diagnosis. Furthermore, the identification of IBS only through ICD-10 codes retrospectively rather than an interview or structures questionnaire may lead to underdiagnosis of IBS, though this would affect both the reference and the exposure groups. In summary, NAFLD was found to be associated with a risk of IBS, and it is important to continue to study modifiable risk factors for IBS given the significant financial burden of the disorder on healthcare systems.
1. In this retrospective study, there was no significant difference in post-operative complications or 30-day readmission rates between patients with a history of prior pelvic or lower abdominal surgery who underwent laparoscopic or open approaches for inguinal hernia repair.
Evidence Rating Level: 2 (Good)
Over 20 million patients undergo surgical repair of their inguinal hernia annually. Prior pelvic or lower abdominal surgery is generally considered to be a contraindication to minimally invasive inguinal hernia repair due to prior scarring and altered pelvic anatomy. However, recent studies have showed that minimally invasive surgery (MIS) for repair of inguinal hernia is safe with experienced surgeons in patients that have undergone previous pelvic or lower abdominal surgery. However, no study has compared the outcomes between open, laparoscopic, and robotic approaches to surgery. This retrospective study aims to compare safety and short-term outcomes of inguinal hernia repair in patients with prior pelvic or lower abdominal surgery. 286 patients with history of prior pelvic or abdominal surgery underwent inguinal hernia repair in the study period at one institution, with 99.5% of surgeries performed by highly experienced hernia surgeons. Overall, 41.6% of patients underwent open surgery, 51.4% underwent laparoscopic surgery, and 7.0% underwent robotic surgery. Demographics were similar between the three groups, but the robotic surgery group had higher BMI and higher rate of prior prostatectomy. When comparing the open repair versus laparoscopic and robotic groups, the open repair group had patients that were significantly older and had a significantly lower BMI. Median days until narcotic cessation and return to activities of daily living were significantly lower in the laparoscopic surgery group compared to open repair. Otherwise, there were no significant differences in post-operative complications or 30-day readmission rates between the three approaches. Of note, there was a similar recurrence rate found between open and laparoscopic repair groups with a similar median follow up. In terms of quality-of-life scores, the open repair group had more pain at 3 weeks post-operatively compared to the laparoscopic and robotic groups as per the Surgical Outcomes Measurement System (SOMS) (P=.008). As per the Carolina Comfort Scale (CCS), there were no significant differences in post-operative pain at 3 weeks, 6 months, and 1 year between the three groups. Overall, the findings from this study are similar to previous studies, showing that MIS hernia repair is safe and effective, even after prior lower abdominal or pelvic surgery in the hands of an experienced surgeon. This study is important to better educate patients about differences between approaches and may shift best practices in surgical hernia repair in the future. A major limitation of this study is that surgeon bias may affect the outcomes given that there was no randomization.
Self-expanding Transcatheter vs Surgical Aortic Valve Replacement in Intermediate-Risk Patients
1. In this randomized clinical trial, there was no significant difference in all-cause mortality or disabling stroke at 5 years between patients who underwent transfemoral transcatheter aortic valve replacement or surgical aortic valve replacement in elderly patents with severe, symptomatic aortic stenosis.
Evidence Rating Level: 1 (Excellent)
Current guidelines recommend that elderly patients with severe, symptomatic aortic stenosis (AS) receive transfemoral transcatheter aortic valve replacement or surgical aortic valve replacement. Multiple previous clinical trials have been performed in elderly patients and have found similar outcomes between surgical aortic valve replacement and TAVR at 2 years post-procedure. However, further research with longer follow-up is important for proper counselling of patients with longer life expectancies. This SURTAVI trial compares outcomes, functional status, and valve performance after self-expanding TAVR or surgery 5 years post-procedure. Patients with sever symptomatic AS at intermediate operative risk were randomized 1:1 to TAVR with supra-annular self-expanding bioprosthesis or surgery, from June 2012 to June 2016 in 87 centers in Canada, Europe, or the United States. Patient assessments were performed at baseline, more frequently within the first year, and annually afterwards, with follow up planned to 10 years. In total, 1669 patients were included in the study, with 864 randomized to TAVR and 796 randomized to surgery. 5 year follow up was available for 603 (93.7%) of patients in the TAVR group and 426 (95.5%) of patients in the surgery group. The primary outcome was all-cause mortality or disabling stroke, occurring in 255 (31.3%) patients that underwent TAVR and 217 (30.8%) that underwent surgery, which was not a significant difference between the two groups. Furthermore, when stratified by revascularization, there was still no significant difference between the two groups. There was, however, a significant difference in valve reintervention, with the TAVR group having a higher incidence of requiring valve reintervention when compared to the surgery cohort (P=.02). With respect to valve performance, patients in the TAVR group had larger orifice areas and lower mean gradients than surgical patients at all time points (P<.001). Otherwise, there was no significant difference in functional improvement or status between the two groups. Overall, this study suggests no difference in all-cause mortality or disabling stroke between patients that received supra-annular self-expanding TAVR and surgical aortic valve replacement in patients with symptomatic severe aortic stenosis at an intermediate surgical risk. Further research into longer follow-ups between the two groups is important for proper counselling and education of patients considering either procedure in the future. Limitations of this study included that given the study population, results may not be applicable to younger patients. Furthermore, results may not be generalized to patients without self-expanding valves, or to patients with procedures performed outside of experienced TAVR centers.
1. In this prospective cohort study, participants with elevated N-terminal pro-B-type natriuretic peptide (NT-proBNP ≥ 450 pg/mL) were found to have similar cardiovascular disease and mortality when compared to participants with prior cardiovascular disease.
2. Participants with an elevated NT-proBNP ≥450 pg/mL have a significantly higher risk of all-cause death and cardiovascular mortality
Evidence Rating Level: 2 (Good)
N-terminal pro-B-type natriuretic peptide (NT-proBNP) is a good predictor of cardiovascular events, particularly heart failure (HF). Currently, guidelines do not recommend the use of cardio biomarkers such as NT-proBNP for clinical decision-making in individuals without overt HF. However, the guidelines do suggest that further evidence about the prognostic value of cardio biomarkers may result in future guideline changes. NT-proBNP elevation may help with risk stratification of patients and help to identify otherwise asymptomatic high risk individuals. This study hypothesizes the existence of a fraction of individuals in the community at high cardiovascular mortality risk without a significant history of disease, that could be identified using NT-proBNP. This study was a prospective cohort analysis from the Atherosclerosis Risk in Communities (ARIC) study. In total, the final group consisted of 9,789 participants aged 54 – 76 years from four communities in the United States. Patients were followed for over twenty years, with a baseline starting in 1996 to 1998. Participants without cardiovascular disease were categorized by NT-proBNP, into <125, 125 – 449, and ≥450 pg/mL. Endpoints analyzed included cardiovascular events such as coronary artery disease, stroke, and heart failure, and participants were followed through until December 2019. With respect to baseline characteristics, 13% of the initial participants had a history of cardiovascular disease, and in comparison, adults in the NT-proBNP ≥450 pg/mL group were older, had a lower BMI, were more likely to be female, white, and more likely to have hypertension, diabetes mellitus, or chronic kidney disease. Overall, there were 4,562 deaths, with higher levels of NT-proBNP being linearly associated with risk of death. Participants with highest NT-proBNP levels were found to have similar or higher rates of cardiovascular disease and mortality compared to those with known cardiovascular disease. In addition, comparing the highest NT-proBNP group (≥450 pg/mL) to the lowest (<125 pg/mL), the highest group had significantly higher risks of all-cause death, cardiovascular mortality, cardiovascular disease, atherosclerotic disease, and heart failure. Overall, results from this study suggest that NT-proBNP elevation is a cardiovascular risk equivalent and is useful for monitoring cardiovascular risk in the community setting. A limitation of this study is that given the participant population, the findings cannot be applied to the general population, but this study is an excellent and promising first step into the use of NT-proBNP for risk stratification.
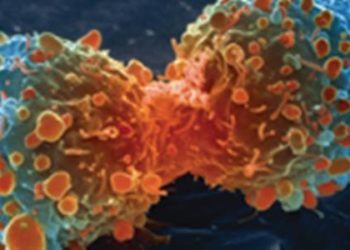
Color or money?: The impact of socioeconomic status and race/ethnicity on breast cancer mortality
1. In this retrospective study conducted in the United States, Black women were found to have a higher 5-year breast cancer mortality rate than White women.
2. Black women in the most prosperous quartile had similar 5-year breast cancer mortality rates when compared to White women in the poorest quartile.
Evidence Rating Level: 2 (Good)
Breast cancer is one of the most common cancers in women and is the second leading cause of cancer-related death in women, only exceeded by lung cancer. The incidence of breast cancer is highest in white women, yet black women experience mortality at a higher rate, a statistic that has persisted despite overall decline in breast cancer mortality. Previous studies have identified biological and socioeconomic factors to explain this discrepancy between different ethnicities; but Hispanic women have been found to have better survival outcomes than white women, who have a higher socioeconomic status. Thus, the aim of this study is to better characterize the impact of race/ethnicity and socioeconomic status on breast cancer mortality in the United States. Data was used from the Surveillance, Epidemiology, and End Results (SSER-18) Program, which covers approximately 28% of the United States population with data from multiple states. Included were female patients with their first primary breast carcinoma diagnosis between 2007 and 2011, who were followed for five years. Demographic data, tumour characteristics, and treatment details were recorded. With respect to socioeconomic status, a ‘prosperity index’ was created, which grouped patients into quartiles, such that the first quartile represents the poorest patients, and the fourth quartile was the most prosperous patients. The primary outcome was 5-year cancer specific survival from diagnosis. In total, 286,520 women were included in the analysis, with 70.1% white women, 10.2% Hispanic women, 11% black women, and the remaining 8.7% of women defined as another race. 71.4% of patients had private insurance or Medicaid, and 75.9% of patients had mastectomy or breast conserving surgery with radiation as the first course of treatment. 49.5% of patients had localized disease at the time of diagnosis. Overall, the 5-year cancer survival rate was 91%. Between white patients and black patients, white patients had a significantly higher 5-year cancer survival rate than black patients (P<.001). With respect to baseline characteristics, white patients were more likely to have private insurance than other races, black patients were less likely to have hormone receptor positive disease, and black patients were more likely to present with metastatic disease. Within each ethnicity, the 5-year survival rate improved as each socioeconomic status quartile became more prosperous. However, black patients had the worst 5-year cancer survival rate at each socioeconomic status quartile. When adjusted for demographics, tumour characteristics, and treatment, black patients in the lowest, second lowest, and third lowest socioeconomic status were found to have a higher risk of 5-year cancer-specific mortality than white patients in the lowest quartile (P<.001). Black patients only in the most prosperous socioeconomic quartile achieved a survival rate that was not significantly difference than white patients in the lowest socioeconomic quartile (P=.211). Thus, the findings of this study suggest that black women have higher 5-year cancer-specific mortality than white women overall, and only the most prosperous quartile of black women have similar mortality rates to the poorest quartile of white women. A major limitation of this study is that patient mortality is not controlled for biological tumour characteristics; future studies that study mortality with controlled biological characteristics would be able to better characterize treatment differences between different ethnicities. This study serves as an important step towards addressing the socioeconomic and racial discrepancies in breast cancer treatment and diagnosis.
Image: PD
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.