2 Minute Medicine Rewind August 4 – August 10, 2014
In this section, we highlight the key high-impact studies, updates, and analyses published in medicine during the past week.
Nutrition deficiency in ICU patients may put them at greater risk for infections and prolong recovery time, however there is controversy over whether supplementing immune-modulating nutrients is beneficial over standard high-protein tube feeds. In this multi-center, double-blind, randomized trial, 301 critically ill adult patients expected to require >72 hours of mechanical ventilation and nutrition were randomized to receive a high-protein formula supplemented with immune-modulating nutrients including glutamine, omega-3 fatty acids, and antioxidants (IMHP) or standard high-protein formula (HP) for up to 28 days to examine impact on incidence of new infections. The incidence of nosocomial infections was similar in the IMHP and HP groups overall (53% vs 52%, p=.96), by type of patient (medical vs surgical vs trauma), or by site of infection. Among medical patients, mortality at 6 months, a secondary outcome, was significantly higher in the IMHP group than the HP group (54% vs 35%, p=.04). Furthermore, after adjustment for age and APACHE-II score, patients receiving IMHP had a 6-month mortality HR of 1.57 compared to the HP group, which is contrary to some smaller prior studies and raises questions about the safety of such supplementation.
Protocols for managing patients suspected of having strokes vary between institutions; some literature suggests centralized stroke care may lead to improved outcomes. Researchers retrospectively analyzed records of 258,915 stroke patients from 2008-2012 in Greater Manchester and London, England, to study the impact of centralizing acute stroke services (which occurred in 2010) on mortality up to 90 days after admission, and hospital length of stay. In London, where all suspected stroke patients were sent to one of a few hyperacute stroke units, mortality decreased by 1% (p=.001), 1.2% (p=.01), and 1% (p=.04) at 3, 30, and 90 days, respectively, compared to stroke mortality in the rest of England, with the greatest decrease in mortality for hemorrhagic strokes (3.3% decrease, p<.006). Hospital stays in London were 1.4 days shorter (p=.003). Comparatively, Greater Manchester, which implemented hyperacute stroke care only for patients presenting within 4 hours of symptom onset, experienced no significant change in stroke mortality vs the rest of England, though hospital stays decreased by 2.1 days (p<.001). These findings support prior evidence that centralized stroke care decrease hospitalization length and may reduce stroke mortality.
As demand for same-day primary care appointments increases, efficient triage of such requests is imperative. In this cluster-randomized trial, 42 practices in the UK that did not already have triage systems in place were randomized 1:1:1 to general practitioner (GP)-led triage, nurse-led triage with computer decision support, or usual care to examine differences in total primary care workload as measured by number of primary care contacts within 28 days of the initial request. Compared to usual care, introducing a GP- or nurse-led triage system resulted in patients receiving significantly more contacts with primary care within a month of an initial call (rate ratio [RR] 1.33, 95%CI 1.30-1.36 for GP-led triage and RR 1.48, 95%CI 1.44-1.52 for nurse triage). GP triage resulted in more telephone calls and fewer in-person appointments, while nurse triage increased nurse telephone time greatly compared to usual care. Despite these differences, hospitalization rates and trial-related mortality were similar across all groups, and overall costs were the same, around £75 at 28 days after the initial request. Patients reported greater satisfaction with usual care or GP triage compared to nurse triage.
Widespread vaccination against human papillomavirus (HPV) has been associated with a reduction in genital warts and high-grade cervical lesions, though a change in HPV prevalence rates after vaccine introduction has not been documented thus far. In this cross-sectional study, HPV prevalence in 268 women in 3 Australian metropolitan areas prior to vaccination implementation (2005-2007) was compared to HPV prevalence in 1058 women from the same geographic areas post-vaccine implementation (2010-2012) to assess overall HPV prevalence andHPV prevalence by strain. Overall HPV prevalence decreased from 60% of women in the pre-vaccination period to 49% in the post-vaccination implementation period (p=.004). Prevalence of HPV infection by vaccine-targeted strains experienced the most significant drop, from 29% to 7% (p<.0001). Decreased prevalence of infection by some HPV strains not targeted by the vaccine was also observed among vaccinated women. Finally, unvaccinated women in the post-vaccination implementation period also had a 10% absolute reduction in the prevalence of vaccine-targeted HPV strains (29% vs 19%, p=.03), suggesting a significant herd immunity effect.
The Trauma and Injury Severity Score (TRISS) for predicting mortality after trauma is often inaccurate when used for elderly patients, and does not account for comorbidities. In this retrospective study, the authors compared TRISS and UHC-EM (University Health Consortium Expected Mortality) predicted mortality to actual mortality for 12,346 non-geriatric and 1743 geriatric trauma patients admitted to a single center from 2005-2012 to evaluate predictive accuracy. Overall, in-hospital mortality after trauma was 18% in geriatric patients vs 6% in non-geriatric patients. The UHC-EM, which models mortality based on both injuries and comorbidities while excluding vital signs data, was more accurate than TRISS in predicting mortality, though both were less accurate in geriatric patients (Area Under the Curve (AUC) 0.93 vs 0.90, p<.05 for non-geriatric patients and AUC 0.89 vs 0.81, p<.05 for geriatric patients).
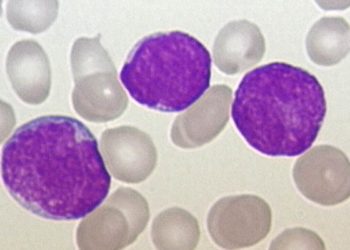
Image: PD/Wiki
©2012-2014 2minutemedicine.com. All rights reserved. No works may be reproduced without written consent from 2minutemedicine.com. Disclaimer: We present factual information directly from peer reviewed medical journals. No post should be construed as medical advice and is not intended as such by the authors or by 2minutemedicine.com. PLEASE SEE A HEALTHCARE PROVIDER IN YOUR AREA IF YOU SEEK MEDICAL ADVICE OF ANY SORT.