2 Minute Medicine Rewind August 8, 2022
Factors Associated With Mortality Among Homeless Older Adults in California
1. Premature mortality was common amongst homeless older adults in the United States.
2. Factors contributing to premature mortality amongst homeless adults included heart disease, cancer, and drug overdose.
Evidence Rating Level: 2 (Good)
Homeless individuals have been known to experience more accelerated aging, premature onset of chronic diseases, impairments in cognition and function, as well as mortality. With the increased overall age of the homeless population in the United States, further research discussing factors contributing to their mortality is vital. This prospective cohort study examined 450 homeless adults older than 50 years of age to assess prevalence, causes, and associated factors of mortality. Participants were interviewed at baseline and follow-up interviews were conducted every six months. The results showed that a total of 26% of participants died through the study timeline and median age at death was 64.6 years. As such, an increased risk of mortality was associated with homelessness over the age of 50 years (aHR 1.62, 95%CI 1.13-2.32). After death certificates of the decedents were analyzed, the most common causes of mortality were found to be heart disease, cancer, and drug overdose. In conclusion, this cohort study confirms that premature mortality is common among homeless older adults. Given these disparities that do exist among this population in the United States as confirmed by this present study, further initiatives to prevent and end the growing homelessness crisis is crucial, especially considering the early mortality in this group. However, this study still has several limitations. For instance, given the small number of deaths that occurred in this study, there may have been a lack in power to detect clear factors associated with mortality. Nevertheless, as premature mortality is likely very common in older homeless adults, there is an urgent need for new policies to address the homelessness endemic in the United States.
1. While patients with Roux-en-Y Gastric Bypass had increased weight loss and higher type 2 diabetes remission compared to sleeve gastrectomy, the variability of effectivity was minimal across race and ethnicity.
2. Racialized patients undergoing RYGB had increased risk of hospitalization, mortality, and major adverse events compared to SG.
Evidence Rating Level: 2 (Good)
While bariatric surgery continues to be very effective for managing severe obesity, various operations differ in long-term safety and effectiveness. As severe obesity is rapidly increasing in prevalence among racialized populations, more research into this area is essential. In this retrospective observational cohort study, 36871 adults and adolescents undergoing a Roux-en-Y Gastric Bypass (RYGB) or sleeve gastrectomy (SG) were included. The outcomes examined include percentage total weight loss, type 2 diabetes remission and relapse, as well as safety and utilization among various racialized groups. The results of this study showed that weight loss was more significant in the RYGB group than SG group (mean difference in percent total weight loss in Black patients was -7.6%, 95%CI -8.0 to -7.1). However, the magnitude of these differences was clinically small amongst different racialized groups. With respect to type 2 diabetes remission, only Hispanic patients were shown to have higher remission rates with RYGB compared to SG (HR 1.19, 95%CI 1.08-1.32). Black, Hispanic, and White patients had higher risk of operation and adverse events at year 5 with RYGB compared to SG (HR 1.45, 95%CI 1.17-1.79; HR 1.48, 95%CI 1.22-1.79; and HR 1.34, 95%CI 1.16-1.54, respectively). As well, risk of all-cause mortality was greater in Hispanic patients compared to other races (HR 2.41, 95%CI 1.24-4.70). In conclusion, this large multicenter cohort study shows that there was increased improvement in weight loss and type 2 diabetes remission in patients who underwent RYGB than SB surgery, with higher rates of adverse events observed in racialized populations. However, this study remains limited as it was not able to identify specific reasons why disparities among various racialized and ethnic groups. Additionally, in this study, more Hispanic and Black patients preferred SG compared to RYGB which may have potentially biased the results. Nevertheless, further research exploring factors involved in these racial differences with regards to outcomes after bariatric surgery can be very useful.
Regular Proton Pump Inhibitor Use and Incident Dementia: Population-Based Cohort Study
1. Regular proton pump inhibitor (PPI) use contributed to an increased incidence for all-caused dementia.
Evidence Rating Level: 2 (Good)
Proton pump inhibitors (PPIs) are commonly used for managing gastric acid-related disorders including gastroesophageal reflux disease (GERD), peptic ulcer disease, and for the eradication of Helicobacter pylori. Several countries promote the purchase of PPIs over the counter, and these are additionally often prescribed in hospitals for incorrect indications and long-term use. Given the increased use of PPIs, more research has been conducted exploring potential adverse effects. However, the association between PPI use and dementia has not been investigated in detail. In this population-based prospective cohort study, 501,002 participants from the UK Biobank were followed for their PPI use, and all-cause dementia. Amongst PPI users, the incident rate of all-cause dementia was 1.06 events per 1000 person-years versus 0.51 events per 1000 person-years among PPI non-users. Individuals who regularly used PPIs were at a greater risk for developing dementia compared to individuals who did not regularly use PPIs (HR 1.20, 95%CI 1.07-1.49). In conclusion, this population-based cohort study showed that regular PPI use was associated with an increased incidence of all-cause dementia, which is consistent with prior research in this field. This study had several strengths including its large sample size and extended follow-up period. However, there were challenges with assessing correct dosage and duration of PPI use which may present a source of bias. As well, only 10% of the total study population used PPI regularly and this was not preassigned to participants. Given various clinical indications for PPI use, it is difficult to determine whether other comorbidities contributed to dementia in individuals using PPIs regularly. Further randomized controlled trials and experimental research can be valuable to assess and confirm the relationship between PPI use and dementia proposed in this study.
1. Frailty status upon admission to intermediate care was a strong predictor of mortality.
Evidence Rating Level: 2 (Good)
Frailty can be defined as a significant reduction in function and health in older adults secondary to a dysregulation in multiple physiological systems. This can have negative implications for health outcomes such as mortality and hospitalization in geriatric populations. Transitions in level of frailty can be further propagated by hospitalization; however, these specific transitions have not been specifically discussed in literature. In this prospective observational study conducted in Spain, 483 participants admitted to intermediate care (IC) facilities were assessed for degree of frailty using a frailty index (Frail-VIG). Degree of frailty was assessed 30 days prior to admission, within 48 hours following admission, at discharge, and 30 days post discharge. The results show that compared to baseline, most patients worsen in frailty after admission. As well, a higher frailty status upon admission was associated with an increased risk of mortality (HR 1.16, 95%CI 1.10-1.22). In conclusion, frailty status changed after admission to intermediate care, and this was a significant predictor for mortality. Further research exploring various factors contributing to worsening frailty amongst hospitalized individuals could be very valuable. However, this study is limited in its methodology. As the focus of this study was on individuals admitted to intermediate care, these findings cannot be generalized to all hospitalized patients. Additionally, frailty is often affected by other factors including socioeconomic status, race, gender, and psychological wellbeing. The effect of these factors on the participants in study were not discussed in detail. Nevertheless, this study provides great insight into frailty and how it can be exacerbated by hospitalizations in elderly patients, ultimately causing poor health outcomes.
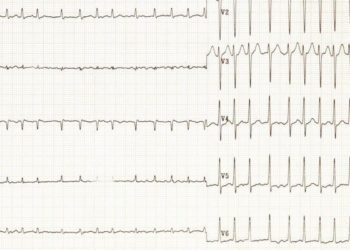
1. A higher physical function among community-dwelling older adults was associated with a decreased risk of cardiovascular disease.
Evidence Rating Level: 2 (Good)
Leading a sedentary lifestyle with minimal physical activity has been shown to be associated with an increased risk of cardiovascular disease. However, there is currently a gap with regards to research investigating individual cardiovascular outcomes amongst older adults in community settings, such as physical activity level. In this community-based prospective cohort study, 5570 participants between 45 and 64 years of age were asked to perform a short physical examination with a wide variety of actions and were assessed for coronary heart disease, stroke, and heart failure. After the physical examination, patients were divided into low, intermediate, and high groups based on their physical function ability. Patients in the low and intermediate scoring categories were more likely to be older in age, female, Black, or have a lower education level. The results of this study show that low and intermediate physical examination groups had an increased risk of cardiovascular disease compared to the high physical examination group (HR 2.41, 95%CI 1.99-2.91 and HR 1.58, 95%CI 1.36-1.84, respectively). In conclusion, amongst older adults living in the community, a lower physical activity score is associated with an elevated risk of developing cardiovascular disease outcomes such as coronary heart disease, stroke, or heart failure. This was independent of pre-existing cardiovascular risk factors. However, there are several limitations that should be discussed in this study. For instance, while the physical activity test had various maneuvers and actions that were tested, a positive performance on this examination may not be an accurate indication of true physical activity level. As well, the study population only consisted of white and black adults so these results cannot be generalizable to other races or age groups. Nevertheless, these findings do demonstrate the importance of physical activity in reducing cardiovascular risk regardless of pre-existing “traditional” risk factors. As such, further research into this area, including randomized trials and experimental studies could be valuable in assessing the exact efficacy of physical function in reducing cardiovascular risk.
Image: PD
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.