2 Minute Medicine Rewind December 16, 2024
Traumatic brain injury and risk of incident comorbidities
1. In this cohort of adults, those who experienced a traumatic brain injury (TBI) of any kind, were associated with a greater risk of developing new treatable medical conditions.
Evidence Rating Level: 1 (Excellent)
Traumatic brain injury (TBI) is a global issue affecting individuals’ quality of life. Previous studies have shown the negative association between TBIs and increased risk of chronic medical conditions. TBI severity was classified based on the Abbreviated Injury Scale for head and neck, ranging from mild TBI (mTBI), to moderate-to-severe TBI (msTBI). This study included the area deprivation index (ADI) score, which is a new area of TBI outcome research. ADI explores the association between neighbourhood disadvantage and postinjury outcomes. The study included patients with TBI and unexposed individuals, all aged 18 years or older when the injury occurred. These individuals were matched using propensity score matching. Individuals were excluded if they had comorbidities of interest. After assessing for eligibility, a total of 20 400 individuals were included, with 5100 patients in the mTBI category (median [IQR] age, 36.0 [25.0-51.0] years), 5100 patients in the msTBI category (median [IQR] age, 25.0 [25.0-52.0] years), and 10 200 matched patients (median [IQR] age, 36.0 [25.0-51.0] years). When separated by ADI score, the lowest quintiles included 2757 unexposed patients (27.0%), 1561 mTBI patients (30.6%), and 1550 msTBI patients (30.4%), whereas in the highest quintiles, there were 1523 unexposed patients (14.9%), 769 mTBI patients (15.1%), and 804 msTBI patients (15.8%). Patients with TBI were associated with a greater risk of all studied conditions compared to patients without TBI. For neurologic disorders, there was an increased risk of seizure disorder (mTBI: HR, 3.24; 95% CI, 2.55-4.11; msTBI: HR, 3.45; 95% CI, 2.73-4.35) and incident dementia (mTBI: HR, 4.06; 95% CI, 3.06-5.39; msTBI: HR, 3.25; 95% CI, 2.43-4.36) in TBI patients compared to the unexposed group. In middle-aged adults, there was an increased risk of suicidality (mTBI: HR, 4.84; 95% CI, 3.01-7.78; msTBI: HR, 4.08; 95% CI, 2.51-6.62), while in older adults there was an increased risk of alcohol misuse and sleep disorders. Overall, this prospective cohort study identified TBI as a risk factor linked to treatable new-onset neuropsychiatric and other medical conditions.
1. In this cohort of individuals with atrial fibrillation (AF), coffee consumption was associated with a higher performance on cognitive tests in a dose-dependent manner, and a decreased presence of inflammatory markers.
Evidence Rating Level: 1 (Excellent)
Atrial fibrillation (AF) is a common heart condition, associated with mild cognitive impairment, and increasing the risk of thromboembolic stroke. Prior epidemiologic studies have suggested a protective effect of regular coffee consumption against cognitive decline. The goal of this observational prospective cohort study was to investigate the association between regular coffee consumption and cognitive impairment in patients with AF. Individuals could be included in the study if they were 65 years of age or older, with a history of AF. Several cognitive assessments were performed including the Montreal Cognitive Assessment (MoCA) questionnaire, the Trail-Making Test (TMT), the Digit Symbol Substitution Test (DSST), and the cognitive construct (CoCo) score. A total of 2413 patients were included (mean age, 73 years), with almost half of the participants drinking 2-3 cups of coffee/day (n=1165, 48.3%). Compared to the control group (-0.24 [95% CI, -0.27 to -0.16), all coffee consumer groups had greater CoCo scores, with the greatest scores achieved by the group with the highest consumption (-0 .10 [95% CI, -0.10 to 0.04; P=0.048]). The results were similar for the MoCA scores, with the lowest scores amongst the control group (24.58 [95% CI, 24.58-25.32]) and the highest scores in the group with the highest coffee intake (25.25 [95% CI, 24.98-26.85; P=0.163]). The presence of inflammatory markers also decreased with increasing coffee intake. Inflammatory markers showed a decrease with increased coffee consumption: hs-CRP (high-sensitivity C-reaction protein) levels were reduced by a factor of 0.78 (95% CI, 0.54-1.13, P=0.188) when consuming ≥5 cups/day compared to <1 cup/day, while IL-6 (interleukin-6) levels decreased by a factor of 0.73 (95% CI, 0.57-0.95, P=0.017). Overall, this prospective cohort study found that in individuals with AF, consuming more coffee was associated with better performance on cognitive tests. Further research is needed to best understand the optimal coffee consumption dose.
1. HbA1C levels were not associated with the number of antibiotic prescriptions in type 2 diabetic patients followed at primary care sites
Evidence Rating Level: 3 (Average)
Diabetes is one of the most common medical conditions worldwide and affected 537 million people worldwide in 2021. Diabetes management focuses on glycemic control through lifestyle interventions (diet and physical activity), oral antidiabetic treatments, insulin use, and the screening/management of microvascular and macrovascular complications. Recent meta-analyses suggest strict glycemic control does not effect the clinically relevant variables of micro- and macrovascular complications. However, there has yet to be consensus on the preventative role of long-term glycemic control on infectious risk. In this retrospective observational cohort study, researchers aimed to address this knowledge gap. Primary care data extracted from the electronic medical records of 1959 patients with T2DM and at least 3 visits were included. Glycemic control was determined by HbA1c values. HbA1c levels were compared to mean antibiotic prescriptions per year. 90.71% of patients with T2Dm were on antidiabetic treatments (65.03% of patients (n = 1274) and insulin treatment in 25.68% (n = 503)). The mean HbA1c was 6.92%. 64% of patients received antibiotic treatments. The most common classes penicillins (51.57%), macrolides (12.46%), streptogramins (9.16%), quinolones (8.73%), and cephalosporins (5%). HbA1c levels were not associated with antibiotic prescriptions but in a multivariate analysis, COPD/asthma was (coefficient 0.60 95% CI [0.383, 0.813] p < 0.001). Cardiac history, the number of antidiabetics, malignancy history, and BMI were statistically independent of antibiotic prescriptions. The number and tupe of antidiabetic treatment also had no impact on antibiotic prescription. Therefore, there was an absence in association between HbA1c levels and antibiotic prescription suggesting diabetic control and infection risk are not linked in T2DM patients followed at primary care centers. Multivariate analysis showed factors that do increase infectious risk are COPD/asthma history and previous antibiotic prescriptions. To bolster this study, patients treated in as hospital inpatients should have been included as they represent patients with more serious infections and potentially more poorly controlled T2DM.
Symptom Recovery in Children Aged 5 to 12 Years With Sport-Related and Non–Sport-Related Concussion
1. Symptom recovery trajectories in children aged 5 to 12 years of age suffering from sport-related concussions (SRCs) and non-sport-related concussions (non-SRCs) were similar, with no significant differences in recovery curves across time postinjury.
Evidence Rating Level: 2 (Good)
Study Rundown: A huge proportion of concussions in young children are associated with sports and recreational activities, which presents a topic of special significance given the fact that the developing brain may be particularly vulnerable to injury. However, previous studies of concussions in children have focused exclusively on SRCs or has combined population samples of children and adolescents rather than focusing on younger children aged 5 to 12 years. This cohort study therefore sought to investigate the similarity in symptom recovery trajectories in children aged 5 to 12 years suffering from SRCs or non-SRCs. In this prospective, multicentre cohort study, 1747 children from 9 pediatric emergency departments in Canada were included and classified as having an SRC or non-SRC if their mechanism of injury occurred outside of a sport setting, such as due to a fall during a recreational activity. The overall cohort was further split into two subcohorts of children aged 5 to 7 and 8 to 12 years of age. Symptoms were assessed via the post-concussion symptom inventory (PCSI) at 1, 2, 4, 8 and 12 weeks post-injury. Among the 1747 children, 513 were aged 5 to 7 (mean [SD] age, 6.57 [0.85] years; 320 male [62.4%]) and 1234 children were aged 8 to 12 years (mean [SD] age, 10.68 [1.40] years; 806 male [65.3%]). No significant differences were observed in recovery trajectories across time postinjury between children in the SRC group and the non-SRC group (5-7 years: β = −0.09; 95% CI, −1.10 to 0.92; 8-12 years: β = 0.11; 95%CI, −1.50 to 1.70). The percentage of patients with PSAC was similar across time for both age groups in the SRC group and the non-SRC group. Overall, this study found that the symptom recovery trajectories in children aged 5 to 12 years of age with SRCs and non-SRCs were similar, with no observed significant differences in recovery curves across time postinjury.
1. In a cohort of adults with inflammatory arthritis, gabapentinoid prescription was associated with an increased risk of fractures.
2. Associations were strongest in patients who more recently were started on gabapentinoids.
3. A similar risk of fracture was found across most doses of gabapentinoids excluding the highest doses.
Inflammatory arthritis (IA) includes various forms of arthritis including rheumatoid arthritis (RA), psoriatic arthritis (PsA), and axial spondyloarthritis (AxSpA). Pain control remains a large challenge in this set of diseases, and often causes significant morbidity. Despite lack of clear evidence suggesting benefit towards pain control, and a host of known side effects such as misuse, fatigue, and respiratory depression, gabapentinoids such as pregabalin and gabapentin remain commonly used for the treatment of IA. In this nested matched case-control study, researchers sought to elucidate whether or not there was an association between fracture risk and gabapentinoid use in patients with IA. National data was utilized from the English primary care and Hospital Episode statistics from the years of 2004 to 2021. 2485 cases met the criteria of having IA and being ever prescribed gabapentinoids, compared to 12,244 controls. It was found that current gabapentoid use was statistically significant with an increased risk of fractures (OR vs. remote: 1.36 [95% CI 1.22, 1.51]), with the most pronounced increase in risk associated with recent prescription in the past 1.65 (1.26, 2.17). The effect was observed to be similar between pregabalin and gabapentin, except in higher doses of gabapentin. Study findings suggest that there may be a statistically significant increase in fracture risk associated with gabapentinoid initiation for the treatment of IA. It is noteworthy however that the clinical significance of said increase remains somewhat unclear, especially in the absence of information on how patient quality of life may otherwise increase via analgesia. Nevertheless, study findings may suggest caution in prescribing gabapentinoids in patients at high risk of falls and fracture, especially given the current paucity of evidence on the efficacy of gabapentinoids for the treatment of IA.
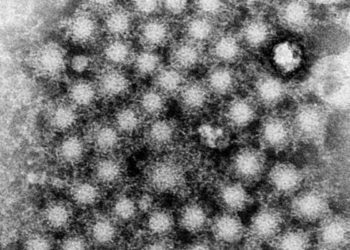
Image: PD
©2024 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.