2 Minute Medicine Rewind December 24, 2018
The optimal duration of androgen suppression therapy with radiotherapy for locally advanced prostate cancer is unknown. In 2018, the French Canadian Prostate Cancer Study (PCS) IV trial showed that 18 months of androgen suppression and radiotherapy is associated with fewer adverse effects than 36 months of the same regimen, suggesting that an even shorten regimen may be safer but still effective. In this randomized, controlled phase 3 trial, 1,071 men with locally advanced prostate cancer at 23 treatment centers across Australia and New Zealand were assigned in a 1:1:1:1 ratio to one of four treatment groups: 6 months of neoadjuvant androgen suppression with leuprorelin and radiotherapy (6AS+RT, control group), an additional 12 months of androgen suppression (18AS+RT), 6AS+RT with 18 months of zoledronic acid, or 18AS+RT with 18 months of zoledronic acid. The primary outcome was prostate cancer-specific mortality, and results were analyzed at 10 years. Omnibus testing for interactions at 10 years revealed that there were no significant differences between androgen suppression and zoledronic acid, and as such, the treatment groups were subsequently collapsed according to duration of androgen suppression and zoledronic acid use. Researchers found that prostate cancer-specific mortality was higher in the 6AS+RT group than in the 18AS+RT group (13.3% vs. 9.7%, respectively, sub-hazard HR (sHR) 0.70, 95% CI 0.50 to 0.98, p=0.035). However, there was no difference in prostate cancer-specific mortality between the no zoledronic acid and zoledronic acid groups (11.7% vs. 11.2%, respectively, sHR 0.95, 95% CI 0.69 to 1.32, p=0.78). There were twelve serious drug-related adverse events. A major limitation of this study was the change in the primary endpoint in 2011 from prostate-specific antigen (PSA) progression to prostate cancer-specific mortality, which compromised the power of the study. Overall, this study suggests that 18 months of androgen suppression plus radiotherapy is safe and more effective than 6 months of the same treatment regimen for locally advanced prostate cancer, but that the addition of zoledronic acid is not beneficial.
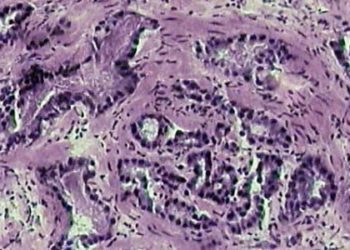
Hepatocellular carcinoma (HCC) is a rapidly increasing cause of morbidity and mortality in patients affected by HIV. However, the impact of HIV infection on HCC prognosis is unclear. Previous studies have provided both null results and evidence of association between HIV and HCC prognosis, but have been characterized by a lack of geographic diversity. In this cohort study, 132 HIV-positive patients and 1,456 HIV-negative patients with untreated HCC from four continents were followed to study overall survival (OS). At baseline, HIV-positive patients were younger (52.9 vs. 66 years, p<0.0001), more commonly male (94.7% vs. 81.9%, p=0.0003), and had a higher prevalence of HCV-related chronic liver disease (78% vs. 37.1%, p<0.0001) compared with patients who were HIV-negative. At the time of HCC diagnosis, most HIV-positive patients were on antiretroviral therapy (64%) and had undetectable HIV RNA levels (52%). Researchers found that HIV infection was independently associated with a 24% greater hazard of death (95% CI 2% to 52%, p=0.0333). Male sex (p=0.0016), Barcelona Clinic Liver Cancer (BCLC) stage, Child-Turcotte-Pugh (CTP) class, alpha-fetoprotein (AFP), and geographical region (all p<0.0001) were also found to be independent prognostic factors. In patients with HIV-infection, AFP (HR 1.18, 95% CI 1.09 to 1.28, p<0.0001) and CTP class C versus A (HR 2.78, 95% CI 1.31 to 5.91, p=0.0079) were both found to be independently associated with OS. This study was limited by the fact that most patients had advanced-stage HCC. Nonetheless, results from this study indicate that HIV infection may adversely influence the clinical course of HCC despite adequate antiretroviral treatment, underlining the need for immunopathologic studies of HIV-associated HCC and additional supports for patients affected by HIV.
Long-term Outcomes of Tetralogy of Fallot: A Study From the Pediatric Cardiac Care Consortium
Tetralogy of Fallot (TOF) is the most common cyanotic heart disease. Surgical repair of TOF was shown in 1954 to have a long-term survival rate of 77%, however, more recent estimates of long-term survival have been biased by selection, differences in treatment strategies, and variation in health care systems. As such, an updated evaluation of long-term survival following TOF repair is needed. In this multicenter retrospective cohort study, 3,283 patients in the Pediatric Cardiac Care Consortium (PCCC) who survived repair for simple TOF were followed up to assess the long-term transplant-free survival of TOF following surgery. Of the study population, 3,168 underwent primary repair, and 762 had a staged approach with initial shunt followed by repair. Researchers found that the long-term transplant-free survival after TOF repair was 98.6%, 97.8%, 97.1%, 95.5%, and 94.5% at 1, 5, 10, 20, and 25 years after repair, respectively. Univariate analysis revealed that staged repair in the early postoperative phase (<6 years) was associated with increased late mortality as compared with primary repair (HR 3.45, 95% CI 2.02 to 5.89), and with non-valve-sparing repair in the early postoperative phase as compared with valve-sparing repair (HR 4.56, 95% CI 1.86 to 11.20). Presence of genetic abnormality was associated with a higher risk of premature mortality in the late postoperative phase (>6 years) (HR 4.41, 95% CI 2.62 to 7.44). Overall, this study showed a very high long-term survival rate after simple TOF repair, and that staged and non-valve sparing operations for TOF were associated with a lower long-term survival rate.
Small for gestational age and risk of childhood mortality: A Swedish population study
Small for gestational age (SGA) fetuses have been shown to have a higher risk of stillbirth and neonatal mortality, but few studies have examined long-term mortality. In this prospective cohort study, 3,795,603 non-malformed singleton live births and 2,781,464 full siblings born between January 1, 1973 and December 31, 2012 were examined to study the association between SGA and all-cause mortality between 28 days and less than 18 years of age. SGA was defined as having a birth weight for gestational age less than the 10th percentile. SGA children were first compared with non-SGA children from the population, then to non-SGA siblings. Of the singleton births, 2.1% were born with severe SGA (<3rd percentile), and 5.7% with moderate SGA (3rd to <10th percentile). Researchers found that age-specific all-cause mortality rates were higher in children with severe SGA than in those with non-SGA in both the population (HR 2.58, 95% CI 2.38 to 2.80) and sibling (HR 2.61, 95% CI 2.19 to 3.10) analyses. The associations were strongest within the period of 28 days to <1 year of age (population-based: HR 4.46, 95% CI 3.98 to 5.00; sibling-based: HR 3.41, 95% CI 2.67 to 4.36). Age-specific all-cause mortality rates were also higher in children with moderate SGA (population-based: HR 1.37, 95% CI 1.28 to 1.47; sibling-based: HR 1.38, 95% CI 1.22 to 1.56). The strongest association of severe SGA with cause-specific mortality was death due to infection (population-based: HR 3.19; sibling-based: HR 4.24). In summary, this study indicates that SGA is associated with an increased risk of childhood death through 18 years of age, and that infection as the most common cause of death.
Neoantigen vaccine generates intratumoral T cell responses in phase Ib glioblastoma trial
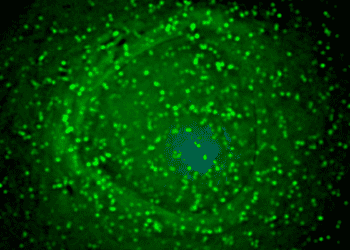
Neoantigens are derived from tumor-specific somatic mutations. As such, they are exempt from immune central tolerance mechanisms and can generate robust immune responses, making them an ideal target for personalized cancer vaccines. Personalized neoantigen vaccination has been previously tested in patients with high-risk melanoma, a cancer that usually harbors a high mutation load. However, the concept has not yet been tested in tumors with a relatively low mutational load, such as glioblastoma (GBM). In this phase I/Ib study, 8 patients with newly diagnosed glioblastoma were immunized with personalized neoantigen vaccines following surgical resection and conventional radiotherapy to assess safety and feasibility. Immune responses were also studied. Vaccines contained up to 20 immunizing neoantigen peptides selected based on whole exome and RNA sequencing of surgically resected GBM and human leukocyte antigen (HLA) class I binding predictions, as well as polyinosinic and polycytidylic acid (poly-ICLC). The median time from surgery to vaccination was 19.9 weeks (range 17.1 to 24.7 weeks), and 6 of 8 patients required dexamethasone therapy during vaccine priming. Five patients did not complete booster vaccinations due to disease progression. Researchers found that patients who did not receive dexamethasone during vaccine priming generated robust de novo tumor-specific immune responses against multiple predicted neoantigens, demonstrated using ex vivo enzyme-linked immunospot (ELISPOT) and ex vivo intracellular cytokine staining assays. Moreover, T-cell receptor (TCR) sequencing and multiplex immunofluorescence revealed that there was an increase in tumor T cell infiltration and tumor-specific TCR clonotypes in these patients. However, patients who required dexamethasone did not generate statistically significant immune responses. Ultimately, all patients died of progressive disease, indicating that vaccine-induced T cell responses did not produce a sufficient anti-tumor response to prevent disease progression. No dose limiting toxicities were observed. Overall, this study suggests that neoantigen vaccination is a feasible therapeutic strategy in tumors with a low mutational burden, and given the success in patients not treated with dexamethasone, future studies will evaluate neoantigen vaccination combined with immune checkpoint blockade for GBM.
Image: PD
©2018 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.