2 Minute Medicine Rewind February 16 – February 22, 2015
In this section, we highlight the key high-impact studies, updates, and analyses published in medicine during the past week.
A Randomized, Controlled Trial of Oral Propranolol in Infantile Hemangioma
Infantile hemangiomas are a common nonmalignant cutaneous tumor of early childhood that can cause significant anxiety in children and their parents. While infantile hemangiomas have a known clinical trajectory with slow resolution, there can be permanent cosmetic sequelae and up to 12% of patients ultimately are referred to specialist management. In this multicenter, randomized control study, 460 infants between 1 to 5 months of age were randomized to either placebo or a 2:2 design of 1 or 3mg/kg of propranolol for 3 or 6 months. A predetermined interim analysis for safety and efficacy was performed after 188 patients received treatment for 24 weeks and demonstrated significant efficacy. There was significantly more complete or near complete resolution in target hemangiomas in patients who received 3mg/kg of propranolol for 6 weeks compared to placebo (60% vs. 4%, p < 0.001) and a majority of patients on propranolol (88%) showed improvement by week 5. There were minimal significant adverse events, however 10% of patients who achieved effect on propranolol had relapse and required retreatment. This study was the first large scale randomized trial of propranolol for the treatment of infantile hemangiomas and suggested the dose of 3mg/kg of propranolol was most effective in its treatment.
The use of corticosteriods is controversial in acute infections. There is conflicting evidence in the intermittent pulse dose steroids in intensive care settings, however there is some evidence for their use in acute bacterial meningitis. The rationale is that severe infections can cause excessive inflammatory responses which can lead to worse outcomes. In this small Spanish randomized controlled trial, 120 patients with community-acquired pneumonia with C-reactive protein (CRP) greater than 150mg/L were randomized to either placebo or 0.5mg/kg of methylprednisolone every 12 hours in addition to usual treatment. Compared to placebo, patients who received methylprednisolone were less likely to progress to a composite endpoint of treatment failure of developing shock, require intubation, radiographic progression, or death (8 patients (13%) vs. 18 patients (31%), p = 0.02). There was not a statistically significant difference in mortality (6 patients (10%) vs. 9 patients (15%), p = 0.37). This early study of corticosteriods in severe community-acquired pneumonia suggests there may be some role of prednisolone in reducing treatment failure.
Mass Treatment with Single-Dose Azithromycin for Yaws
Yaws is a tropic infection of Treponema pallidum pertenue resulting in skin lesions and destructive lesions of the bone. Efforts by the World Health Organization in the mid-last century reduced the global incidence of yaws by 95% through the use of intramuscular penicillin. Current efforts to eradicate the disease utilizes a once-dose of oral azithromycin of all members of a community in endemic areas. In this longitudinal study from April 2013 to May 2014, investigators used this current approach in Lihir Island, an island of 28 villages with 16,092 inhabitants with endemic yaws. The prevalence of active yaws was 2.4% prior to mass treatment. During the first step, 82.7% of residents received a dose of azithromycin and the prevalence of active yaws decreased to 0.3% (p<0.001) at 12 month follow-up. There was no evidence of resistence, however 17% of participants endorsed medication side effects including nausea, vomiting, and diarrhea within one week. This study in Papua New Guinea suggests oral azithromycin is effective in current strategies to eliminate yaws.
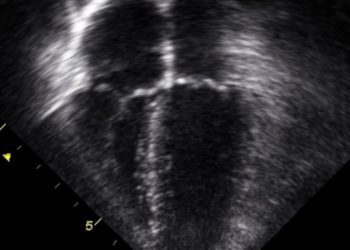
The International Subarachnoid Aneurysm Trial (ISAT) enrolled patients from September 1994 to May 2002 to assess the comparative efficacy of neurosurgical clipping with endovascular coiling for the treatment of ruptured cerebral aneurysms. The initial results suggested that at one year, there was a mortality benefit and improvement in neurological outcomes by endovascular coiling, however the durability of the result was questioned and it was suggested patients who underwent endovascular coiling were more likely to require re-treatment. In this report of long term outcomes, investigators report the outcomes of 1644 patients enrolled from 22 centers from the United Kingdom who had follow-up for between 5 and 14 years. At ten years, 83% of patients who underwent endovascular clipping and 79% of patients who underwent neurosurgical clipping were still alive (adjusted OR 1.35, 95% CI: 1.06 – 1.73). The majority of patients had low modified Rankin scores (0-2) (82% in the endovascular coiling group vs. 78% with neurosurgical clipping. OR 1.25, 95% CI 0.92-1.71). Long term follow-up suggests that there was durable improvement from endovascular coiling over neurosurgical clipping in the probablity of death or having significant neurological impairment.
Image: PD
©2015 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.