2 Minute Medicine Rewind January 19 – January 25, 2015
In this section, we highlight the key high-impact studies, updates, and analyses published in medicine during the past week.
The reference limit for cardiac troponin levels in defining myocardial infarction (MI) is currently the same for men and women, however troponin levels vary significantly by sex, with the 99th percentile level being twice as high in men compared to women, potentially resulting in the under-diagnosis of MI in women. In this single-center, prospective cohort study, investigators obtained standard and high sensitivity troponin I studies in 1126 consecutive patients (45% women) suspected of having an acute coronary event to determine the effect of a high sensitivity troponin assay with sex-specific thresholds on MI diagnosis rates among men and women. The rate of diagnosis of Type 1 MI (myocardial ischemia thought to be due to acute coronary syndrome) was nearly doubled in females (22% vs 11%, p<.001) when using a high sensitivity assay with sex-specific troponin threshold compared to a contemporary assay using a single threshold. Women identified as having an MI by the high sensitivity assay and sex-specific threshold had a 25% risk of death or recurrent MI within 12 months of follow-up, similar to those diagnosed with MI using both assays (24% risk), much higher than those who were determined not to have an MI by either method (4% risk). By contrast, the rate of Type 1 MI increased only slightly, though significantly, among men compared to the standard assay and threshold (21% vs 19%, p=0.002). These results suggest that myocardial infarction is under-diagnosed in women and results in subsequent inequalities in management and follow-up.
There is concern that trends in increased sedentary time may contribute to adverse health outcomes independent of time spent engaged in physical activity. In this systematic review and meta-analysis, authors identified 47 studies assessing sedentary time and health outcomes after adjusting for physical activity. Increased sedentary time was independently associated with an increased risk of all health outcomes, including all-cause mortality (HR 1.24, 95%CI 1.09-1.41), Type 2 diabetes (HR 1.91, 95%CI 1.65-2.22), cardiovascular disease incidence (HR 1.14, 95%CI 1.00-1.30), cardiovascular disease mortality (HR 1.18, 95%CI 1.11-1.24), cancer incidence (HR 1.13, 95%CI 1.05-1.21), and cancer mortality (HR 1.16, 95%CI 1.10-1.22). Furthermore, analysis of 10 studies that examined the pooled effects of sedentary time, physical activity, and all-cause mortality revealed a 30% decrease in all-cause mortality for those with high vs low levels of physical activity with similarly high amounts of sedentary behavior (HR 1.16, 95%CI 0.84-1.59 vs HR 1.46, 95%CI 1.22-1.75). These results suggest that efforts to reduce sedentary time, which is not a current public health focus, will yield additional health benefits independent of increasing physical activity.
Causes and Timing of Death in Extremely Premature Infants from 2000 to 2011
Changes in care for premature infants has led to improved survival, though trends in the causes of death have not been examined on a large scale. In this multicenter cohort study, researchers compared data from the deaths of 6075 extremely premature infants (22 through 28 weeks gestation) separated into 3 cohorts from 2000-2011 to determine trends in overall mortality and to compare the causes and timing of death among these groups. Overall in-hospital mortality decreased from 285 to 258 per 1000 live births between the 2000-2003 cohort and the 2008-2011 cohort (p=.003 for trend among 3 periods), with a decrease in pulmonary causes of death accounting for 53% of overall change (from 83 to 68 deaths per 1000, p=.002). Deaths related to infection or CNS injury also showed a significant downward trend. On the other hand, deaths attributed to necrotizing enterocolitis increased from 23 to 30 per 1000 live births from the first to third cohort (p=.04). This increase may be due to improvements in neonatal care resulting in the survival of infants who would otherwise have died before necrotizing enterocolitis could have developed.
Chlorhexidine Bathing and Health Care-Associated Infections: A Randomized Clinical Trial
Chlorhexidine bathing may reduce the bacterial burden of skin flora and thereby reduce hospital-acquired infections and is practiced widely, though its effect on various types of infections is unclear. In this single-center cluster-randomized, crossover trial, researchers analyzed records of 10,783 patients in each of 5 ICUs assigned to bathe patients daily using 2% chlorhexidine wipes or nonantimicrobial cloths for 10 weeks followed by 3 crossovers, such that each ICU used each bathing method twice, separated by 2-week washout periods. The primary outcome of health care-associated infections (composite of central line infections, catheter-associated urinary tract infections, ventilator-associated pneumonia, and C.difficile infection) was no different between the chlorhexidine and control groups (55 vs 60 infections, or 2.86 vs 2.90 infections per 1000 patient-days, respectively, p=0.95; adjusted RR 0.94, 95%CI 0.65-1.37, p=0.83). Similarly, no difference in infection rate between the groups was found when examining infection types separately. The results of this study contradict a prior multi-center randomized trial which found that chlorhexidine bathing reduced MRSA and VRE colonization and bloodstream infections and suggest the practice of routine chlorhexidine bathing of critically ill patients is not supported.
High dietary sodium intake is associated with hypertension, a main risk factor for cardiovascular disease, however restrictive sodium intake has recently been shown to have adverse effects and is now controversial. In the 10-year follow-up of this prospective cohort study, researchers analyzed long term follow-up data from 2642 adults between ages 71-80 as stratified by dietary sodium intake from initial survey. The investigators found that sodium intake level was not associated with overall mortality (HR per 1g extra of sodium: 1.03, 95% CI 0.98 – 1.09, p = 0.27), cardiovascular disease (HR per 1g extra of sodium: 1.03, 95% CI 0.95 – 1.11, p = 0.47), no heart failure (HR per 1g extra of sodium: 1.00, 95% CI 0.92 – 1.08, p = 0.92). Adjustment for caloric intake, body mass index, sex, race, or hypertensive status did not affect conclusions. The intermediate sodium intake group (1.5g/d – 2.3g/d) had the lowest mortality, with non-statistically significant differences in 10-year mortality in the groups with less and more sodium intake. There was no significant impact on mortality, cardiovascular disease risk, or heart failure risk by patient’s baseline survey on sodium intake.
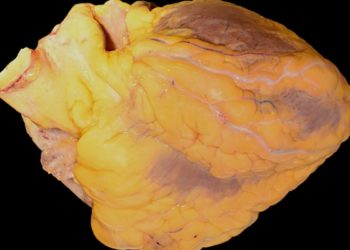
Image: PD
©2014 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. No article should be construed as medical advice and is not intended as such by the authors, editors, staff or by 2 Minute Medicine, Inc.