2 Minute Medicine Rewind January 4 – January 11, 2015
In this section, we highlight the key high-impact studies, updates, and analyses published in medicine during the past week.
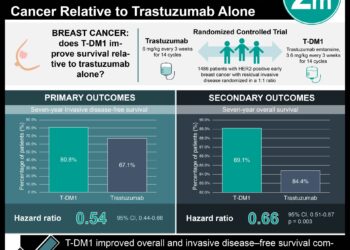
Adjuvant Paclitaxel and Trastuzumab for Node-Negative, HER2-Positive Breast Cancer
Trastuzumab has been shown to be an effective therapy for Stage II and III HER2-positive breast cancers in multiple large trials. However, whether the benefits of this drug outweigh its toxicities in Stage I HER2-positive breast cancer remains unstudied. IN this uncontrolled, single-group study, 406 patients with HER2-positive breast cancer tumors less than 3 cm were treated with paclitaxel and trastuzumab for 12 weeks followed by 9 months of trastuzumab monotherapy. Researchers found that at 3 years 98.7% (95% CI 97.6-99.8) of patients were free from invasive disease. This is in contrast to past studies of other treatment regimens that have shown recurrence rates of 3-50%. With respect to adverse events, 3.2% (95% CI 1.7-5.4) of patients reported at least one episode of grade 3 neuropathy, 0.5% (95% CI 0.1-1.8) had symptomatic congestive heart failure, 3.2% (95% CI 1.7-5.4) had significant asymptomatic declines in ejection fraction. The heart failure effects resolved upon discontinuation of trastuzumab. This study therefore shows that among women with predominantly stage I HER2-positive breast cancer, adjuvant paxlitaxel plus trastuzumab results in a recurrence rate of 2% at 3 years with a relatively low rate of serious adverse events.
TBX6 Null Variants and a Common Hypomorphic Allele in Congenital Scoliosis
Congenital scoliosis affects an estimated 1 in 2000 live births. However, the genetic basis for this disease has yet to be thoroughly understood. Extrapolating from previous animal studies, researchers in this genetic study searched for a 16p11.2 deletion affecting theTBX6 gene in 161 individuals with congenital scoliosis and compared it with 166 patient controls. Investigators identified the 16p11.2 mutation in 11% of the patients but in none of the controls (p < 3.8E-6). Using pedigree analysis, scientists additionally found that a common hypomorphic TBX6 haplotype was a necessary second risk allele that was seen in all carriers of the TBX6 null mutation. The presence of both the TBX6 null mutation and the hypomorphic TBX6 allele was necessary for the scoliosis phenotype, a finding that was re-confirmed in an additional cohort of 76 patients with congenital scoliosis. This study therefore provides the first evidence that compound inheritance of a null and hypomorphic mutation of the TBX6 gene accounts for a significant portion of congenital scoliosis cases.
Association Between 7 Years of Intensive Treatment of Type 1 Diabetes and Long-term Mortality
The Diabetes Control and Complications Trial (DCCT) from 1983-1993 showed that tighter glucose control had improved outcomes over conventional therapy at the time. This paper summarizes the long-term outcomes for the patients from this trial. During the initial trial, 711 patients with Type 1 diabetes were assigned to receive intensive therapy with an average HbA1c of 7% after a median follow-up of 6.5 years. 730 patients were randomized to conventional therapy and had an average HbA1c of 9% after a median follow-up of 6.5 years. Investigators were able to follow up on 99.2% of participants after a mean time of 27 years. They found that there was a lower all-cause mortality risk in the intensive therapy group (HR 0.67, 95% CI 0.46-0.99, p = 0.045). Higher HbA1c levels were associated with increased all-cause mortality (HR 1.56, 95% CI 1.35-1.801, per 10% relative increase in HbA1c) and the development of albuminuria (HR 2.20, 95% CI 1.46-2.21, p < 0.001). This study therefore shows that after 27 years, intensive diabetes therapy for at least 6.5 years was associated with a modestly lower all-cause mortality rate compared with conventional therapy.
HIV positive patients are known to have a higher risk of myocardial infarction. However, the role of statin therapy in reducing cardiovascular risk in these patients is unknown. In this randomized control trial, 40 HIV positive patients with sublinical coronary atherosclerosis, arterial inflammation in the aorta seen on FDG-PET, and LDL < 130mg/dL were randomized to either atorvastatin or placebo. Researchers found that among the 21 patients who could be assessed after 12 months by FDG-PET, there was no significant difference in inflammation of the aorta between the groups (atorvastatin Δ −0.03, 95% CI −0.17-0.12 vs. placebo Δ −0.06, −0.25-0.13, p=0.77). Among all 37 patients, there was a significant decrease in non-calcified coronary plaque volume in the intervention group compared to the control group (-19.4%, IQR -39.2-9.3 vs -20.4%, IQR -7.1-94.4, p = 0.009). The number of high-risk plaques was also reduced: -0.2 (95% CI -0.6-0.2) low attenuation plaques vs. 0.4 (0.0-0.7) (p=0.03) and -0.2 (-0.4-0.1) positively remodeled plaques vs. 0.4 (−0.1-0.8) (p=0.04) for the intervention and control groups respectively. LDL levels were also significantly decreased in the statin group compared with the placebo group (-1.00 mmol/L, 95% CI -1.38-0.61 vs. 0.30 mmol/L, 95% CI 0.04-0.55, p<0.001). There was a low incidence of adverse events. This study shows that while there was no observable, statistically significant improvement in arterial inflammation, statin therapy in HIV positive patients did reduce the number and volume of high-risk coronary plaques.
Whether statins are equally effective for primary prevention in women as in men is not thoroughly understood. In this meta-analysis, investigators pooled data from 27 trials and found that 46,675 women participated in these trials, representing 27% of studied patients. Women experienced the same reduction in 1-year lipid concentrations as men and generally also had the same outcomes. When comparing women to men, women had a rate ratio of 0.84 for major vascular events (99% CI 0.78-0.91) compared to 0.78 for men (0.75-0.81)(p = 0.33). Similarly, the reductions in major coronary events, coronary revascularization, and stroke were not statistically different between the sexes. Overall the all-cause mortality reduction with statin therapy was also similar (RR 0.91, 99% CI 0.84-0.99 in women vs. 0.90, 0.86-0.95 in men, p = 0.43). This study therefore shows that statin therapy does not appear to have a difference in preventing major vascular events in women versus men.
Image: PD
©2015 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. No article should be construed as medical advice and is not intended as such by the authors, editors, staff or by 2 Minute Medicine, Inc.