2 Minute Medicine Rewind July 1, 2024
Multivitamin Use and Mortality Risk in 3 Prospective US Cohorts
1. In a cohort of healthy adults, multivitamin use was not associated with lower mortality risk at 20 years follow-up.
Evidence Rating Level: 2 (Good)
Approximately one-third of adults in the United States (US) use multivitamins (MV) to maintain or improve health and prevent chronic disease. However, the association between MV use and mortality have been mixed. This cohort study evaluated how self-reported daily MV use was associated with mortality risk in generally healthy adults. Data from three prospective cohort studies in the United States, with follow-up periods of over 20 years were analyzed. Analyses were performed for the first 12 years of follow-up (follow-up period 1 (FP1)) and the last 15 years of follow-up (follow-up period 2 (FP2)). Among 390,124 participants without a history of major chronic diseases (median [IQR] age, 61.5 [56.7-66.0] years; 21,6202 [55.4%] male), there was no association between MV use and lower all-cause mortality risk in FP1 (multivariable-adjusted hazard ratios (HRs) 1.04; 95% CI, 1.02-1.07), nor FP2 (multivariable-adjusted HR, 1.04; 95% CI, 0.99-1.08). In contrast, daily MV users had a 4% higher mortality risk than nonusers (FP1: HR, 1.04; 95% CI, 1.02-1.07; FP2: HR, 1.04; 95% CI, 0.99-1.08). Although this study did not find regular MV use among US adults to improve longevity, the authors did not rule out the possibility that daily MV use may relate to other health outcomes associated with aging. Overall however, study findings suggest that there is no long term mortality benefit associated with multivitamin use.
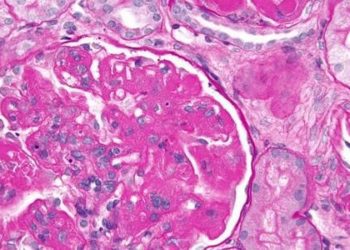
1. Unhealthy sleep, as well elevations of liver enzymes and decreased levels of albumin and liver functional biomarkers, were significantly associated with increased risk of liver cancer.
Evidence Rating Level: 2 (Good)
Poor sleep quality has been positively associated with cancer risk; however, the association between sleep and liver cancer risk specifically remains unclear. Studies examining routine liver function biomarkers and the risk of incident liver cancer in the general population with large sample sizes are also limited. Such liver function biomarkers include alanine transaminase (ALT), aspartate transaminase (AST), gamma-glutamyl transferase (GGT), albumin (ALB), alkaline phosphatase (ALP), total bilirubin (TBIL), and total protein (TP). This study thus investigated the separate and joint effects of sleep and liver function biomarkers on liver cancer using data from the UK Biobank, a prospective cohort recruited from 22 centers around the UK. Five sleep traits including sleep duration, morning/evening chronotype, insomnia, snoring, and excessive daytime sleepiness were used to create sleep scores that divide participants into either “healthy sleep” or “unhealthy sleep” categories. A total of 356, 894 participants were included in the study (mean age = 62±9 years, male N (%) = 170,831 (47.87%), mean BMI = 27.40 ± 4.73 kg/m2) and the median follow-up time was 13.1 years. Unhealthy sleep (vs healthy sleep) was associated with a 46% increased risk of liver cancer incidence (multivariable-adjusted hazard ratio (HR) 95% CI = 1.46 (1.15–1.85). Liver cancer risk was also associated with higher levels of ALT, AST, TBIL, GGT, ALP, or TP, and lower levels of ALB (HRs (95% CI): ALT = 1.17 (1.15–1.20), AST = 1.20 (1.18–1.22), TBIL = 1.69 (1.47–1.93), GGT = 1.06 (1.06–1.07), ALP = 1.08 (1.07–1.09), TP = 1.81 (1.37–2.39), ALB = 0.29 (0.18–0.46)). The highest risk for liver cancer was observed for individuals with unhealthy sleep and high (≥ median) ALT, AST, TBIL, GGT, ALP, or TP or low (< median) ALB level (HRs 95% CI: ALT = 3.65 (2.43–5.48), AST = 4.03 (2.69–6.03), TBIL = 1.97 (1.40– 2.77), GGT = 4.69 (2.98–7.37), ALP = 2.51 (1.75–3.59), TP = 2.09 (1.51–2.89), or ALB = 2.22 (1.55–3.17). Unhealthy sleep with high TP levels had a significant additive interaction on liver cancer with relative excess risk due to an interaction of 0.80 (0.19–1.41). Overall, the study results suggest that healthy sleep and controlling liver function biomarker levels may reduce the risk of liver cancer.
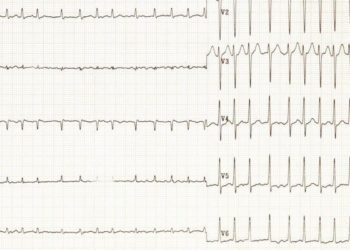
1. Among US cancer survivors, metformin was associated with a lower risk of cardiometabolic diseases, all-cause mortality, and cardiometabolic mortality.
Evidence Rating Level: 1 (Excellent)
Cardiometabolic disease (CMD) is the leading cause of noncancer deaths in the cancer survivor (CS) population. Previous studies have found metformin to improve cardiometabolic status in populations with obesity, diabetes, or psychiatric disorders, potentially by inhibiting oxidative stress. However, the relationship between metformin use and cardiometabolic status in the CS population is limited. This prospective cohort study thus examined the association between metformin use and the risk of CMD / CMD-related mortality, as well as the role of the antioxidative stress mechanism in cancer survivors enrolled in the National Health and Nutrition Examination Survey. Among 3995 cancer survivors (weighted population = 21,671,061, weighted mean [SE] age = 62.62 [0.33] years; females = 2119 [53.04%]), 448 reported metformin usage. During the follow-up period of up to 17 years (median, 6.42 years), there were 1233 recorded deaths, 481 of which were from cardiometabolic causes. In the overall population of cancer survivors, metformin use was associated with a lower risk of all-cause (hazard ratio [HR] = 0.62; 95% CI, 0.47–0.81) and cardiometabolic (HR, 0.65; 95% CI, 0.44–0.97) mortality compared with metformin nonusers. Metformin use also correlated with a lower risk of total cardiovascular disease (odds ratio [OR], 0.41; 95% CI, 0.28–0.59), stroke (OR, 0.44; 95% CI, 0.26–0.74), hypertension (OR, 0.27; 95% CI, 0.14–0.52), and coronary heart disease (OR, 0.41; 95% CI, 0.21–0.78). These inverse associations, specifically metformin use and total CVD risk were also observed in patients with four specific cancer types identified as cardiometabolic high-risk, which included hematologic (OR, 0.29; 95% CI, 0.17–0.50), breast (OR, 0.42; 95% CI, 0.27-0.64), colorectal (OR, 0.32, 95% CI, 0.17-0.63) and prostate cancer (OR, 0.54; 95% CI 0.30-0.98). Individuals in the no metformin usage and high oxidative stress (OS) category displayed the highest risks of all-cause/cardiometabolic mortality and CMD, suggesting that metformin may antagonize oxidative stress. Overall, this study found that metformin use was associated with reduced risks of all-cause mortality, cardiometabolic disease, and associated mortality. Longitudinal studies are warranted to determine the practical application and pharmacological mechanisms of metformin in managing cardiometabolic health among the CS population.
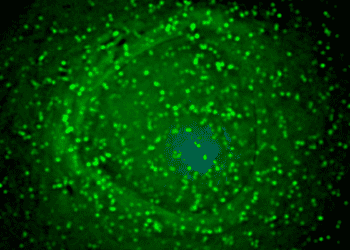
1. Serum IL-1β and IL-6 levels were higher in OCD patients compared to healthy controls.
Evidence Rating Level: 3 (Average)
Emerging evidence suggests immune dysregulation to be involved in the pathogenesis of obsessive-compulsive disorder (OCD). Interleukin-1β (IL-1β) and interleukin-6 (IL-6) are crucial pro-inflammatory cytokines for regulating immune responses; however, their role in OCD is unclear. This case-control study of 58 OCD patients and 30 age-sex-matched healthy controls (HCs) (mean age = 32.14±1.43, male N (%) 34 (58.62%), mean BMI = 23.97±0.62 kg/m2) thus examined the role of IL-1β and IL-6 in the pathophysiology of OCD. Compared to the HCs, OCD patients had higher serum IL-1β levels (23.68±1.65 pg/ml vs. 15.75±1.02 pg/ml; p = 0.002) and higher serum IL-6 levels (44.97±0.73 pg/ml vs. 37.04±0.35 pg/ml; p<0.001). While elevated IL-6 levels were maintained for both sexes individually in OCD patients compared to HCs (p < 0.001), IL-1β serum levels were maintained only in male OCD patients (p = 0.006). Serum IL-1β (r = 0.380, p = 0.015) and IL-6 levels (r = 0.324, p = 0.026) were both significantly associated with greater scores on the Yale-Brown Obsessive Compulsive Scale (Y-BOCS), reflecting greater severity of OCD symptoms. Overall, study results suggest that serum IL-1β and IL-6 levels may be involved in OCD pathogenesis and could potentially serve as blood-based biomarkers for OCD risk assessment. Future studies with larger sample sizes are warranted.
Hip Fracture Risk Assessment Tools for Adults Aged 80 Years and Older
1. Femoral neck bone mineral density (FNBMD) alone discriminated 5-year hip fracture risk at least as well as FRAX and Garvan tools incorporating FNBMD.
2. Fracture Risk Assessment Tool (FRAX) modestly underpredicted observed hip fracture probability in intermediate-risk individuals and Garvan greatly overpredicted observed hip fracture probability in high-risk individuals.
Evidence Rating Level: 2 (Good)
Adults 80 years and older make up 70% of hip fractures in the United States. Tools to estimate absolute risk of hip fracture include the Fracture Risk Assessment Tool (FRAX) and Garvan fracture risk calculator. However, it is unclear how well these tools perform in predicting hip fracture in late life when competing mortality risks may be prevalent. Using data from 3 prospective cohort studies, this study compared the performance of the FRAX, Garvan Fracture Risk Calculator, and femoral neck bone mineral density (FNBMD) alone in 5-year hip fracture prediction in adults 80 and over. Among 8890 participants (mean age = 82.6 + 2.7 years; women = 4906 (55.2%)), 321 women (6.5%) and 123 men (3.1%) experienced a hip fracture; 818 women (16.7%) and 921 men (23.1%) died before hip fracture during the 5-year follow-up. Among women, area under receiver operating characteristic curve (AUC) was 0.69 (95% CI, 0.67-0.72) for FRAX, 0.69 (95% CI, 0.66-0.72) for Garvan, and 0.72 (95% CI, 0.69-0.75) for FNBMD alone. FNBMD alone was superior to both FRAX (P = .01) and Garvan (P = .01) in hip fracture discrimination in women. Among men, AUC was 0.71 (95% CI, 0.66-0.75) for FRAX, 0.76 (95% CI, 0.72-0.81) for Garvan, and 0.77 (95% CI, 0.72-0.81) for FNBMD alone. Both Garvan and FNBMD alone were superior to FRAX (P < .001) in hip fracture discrimination in men. Among both sexes, Garvan greatly overestimated 5-year hip fracture probability among individuals in upper quintiles of predicted risk, while FRAX modestly underestimated risk among those in intermediate quintiles of predicted risk. Overall, until improved risk prediction tools are available, study results suggest clinicians should prioritize consideration of hip BMD, life expectancy, and patient preferences when deciding on drug treatment initiation for hip fracture prevention in adults 80 years and older.
Image: PD
©2024 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.