2 Minute Medicine Rewind July 17, 2023
Results following implementation of a cardiac surgery ERAS protocol
1. Postoperative enhanced recovery after surgery (ERAS) protocols for cardiac surgeries were found to improve outcomes such as decreasing the length of stay (LOS) and incidences of postoperative infections.
2. There was a significantly reduced 30-day mortality for patients who underwent open aortic surgeries after the implementation of ERAS protocols, compared to the pre-implementation cohort.
Evidence Rating Level: 2 (Good)
ERAS protocols provide guidelines for standardized perioperative pathways that aim to optimize patient care. In the field of cardiac surgery, the adoption of ERAS protocols has faced resistance due to the complexity of operations, acuity of patients, and paucity of literature surrounding its implementation. At Standford Hospital, ERAS post-operative care pathways for Coronary artery bypass graft (CABG)/Valve and Aortic surgeries have been established. This single-center retrospective cohort study aims to examine the impact of these protocols by comparing outcomes in the post-pathway implementation cohort with those who received care prior to implementation. For the CABG/Valve pathway, a total of 747 patients were propensity matched in the pre-and post-implementation cohorts. While there was no significant improvement in 30-day mortality, the post-implementation cohort had a significant decrease in the post-op LOS (7.0 vs. 6.0 days, p<0.001) and median ICU LOS (54.0 vs. 69.9 hours, p<0.001) compared to the pre-implementation cohort. Among other improvements like decreased duration of mechanical ventilation and faster return to ambulation, notably, there was also a decreased incidence of post-op ventilator-associated pneumonia (VAP) (p=0.003) and post-op urinary tract infections (UTIs) (p<0.001). For the Aortic Procedure pathway, a total of 586 patients were propensity-matched in the pre-and post-implementation cohorts. In contrast to the CABG/Valve cohorts, there was a significant decrease in 30-day mortality from 7% in the pre-implementation cohort to 3.5% in the post-implementation cohort (p=0.012), but no significant improvement in post-op or ICU LOS. While there was a significant decrease in the duration of mechanical ventilation and a significantly faster return to ambulation, there was no significant difference in the incidence of postop UTIs or VAPs. Overall, this study demonstrates that the implementation of ERAS protocols for cardiac surgeries at Standford Hospital decreases morbidity and LOS, and improves mortality for more critically ill patients who underwent open aortic operations.
1. For obese patients with minor stroke or transient ischemic attacks (TIA), subsequent therapy with ticagrelor-acetylsalicylic acid (ASA) was associated with lower risk of subsequent stroke compared to clopidogrel-ASA.
2. This difference in risk reduction was not observed in nonobese patients.
Evidence Rating Level: 1 (Excellent)
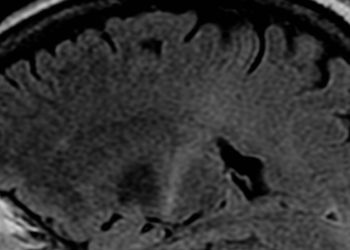
The treatment of patients with minor ischemic stroke and TIA with dual antiplatelet therapy, namely clopidogrel and ASA or with ticagrelor and ASA, is well established as efficacious. In the Ticagrelor or Clopidogrel with Aspirin in High-Risk Patients with Acute Nondisabling Cerebrovascular Events II (CHANCE-2) trial, ticagrelor-ASA therapy was more effective in reducing stroke risk compared to clopidogrel-ASA therapy in patients with minor ischemic stroke or TIA who carried CYP2C19 loss-of-function alleles. However, various factors, including obesity, can influence the efficacy of antiplatelet therapy. Therefore, this secondary analysis of the 6412 patients enrolled in the randomized, double-blind, multicentre CHANCE-2 trial aimed to evaluate the efficacy and safety of ticagrelor-ASA and clopidogrel-ASA as stratified by BMI. Patients diagnosed with an acute minor ischemic stroke or a high-risk TIA were randomly assigned in a 1:1 ratio within 24 hours of symptom onset to the ticagrelor-ASA group (n=3205) or clopidogrel-ASA group (n=3207). Patients with a BMI ≥ 28 (n=876, 13.7%) were classified as obese, while those with BMI < 24 and 24-28 were nonobese (n=5536, 86.3%). For each 5-unit increase in BMI, the hazard ratio (HR) of 90-day stroke with ticagrelor-ASA therapy, compared to clopidogrel-ASA, decreased by 17.98% (95% CI 17.97%-18.00%). Furthermore, compared with the clopidogrel-ASA group, ticagrelor–ASA had a significantly lower rate of stroke within 90 days in patients with obesity (HR 0.51, 95% CI 0.30–0.87), but not in nonobese patients (HR 0.84, 95% CI 0.69–1.04). The interaction between the treatment group and BMI was significant (p=0.04). Overall, these findings suggest that obese patients with minor ischemic stroke or TIA who are carriers of CYP2C19 loss-of-function alleles, experience a greater clinical benefit from ticagrelor–ASA therapy than with clopidogrel–ASA therapy.
1. Internet-delivered emotion regulation for adolescents (IERITA) used in combination with treatment as usual (TAU) produces larger reductions in nonsuicidal self-injury (NSSI) frequency and improves emotion dysregulation.
Evidence Rating Level:1 (Excellent)
NSSI, affecting 3% to 7% of adolescents, refers to deliberate harm to one’s body without suicidal intent and is a significant risk factor for suicide attempts. There are limited empirically supported and accessible treatments for NSSI in adolescence. Emotional dysregulation has been identified as a key mechanism underlying NSSI, therefore IERITA has been proposed as a treatment for NSSI. This 3-site, single-masked, randomized superiority clinical trial aimed to investigate the effectiveness of therapist-guided IERITA as an adjunct to treatment as usual (TAU) compared to TAU alone. Therapist-guided IERITA comprised 11 modules for adolescents and 6 modules for parents delivered over 12 weeks, with a dedicated therapist providing online support via a message function. TAU typically involved supportive therapy sessions every 2 weeks with community clinicians. A total of 166 participants (mean [SD] age, 15.0 [1.2] years; 92.8% female) were recruited between November 2017 and April 2020, and were randomly allocated to receive therapist-guided IERITA plus TAU (84 participants) or TAU alone (82 participants). There was a significantly larger reduction in both self-reported and masked assessor-rated NSSI frequency in the IERITA plus TAU vs TAU only group, at both the 1-month and 3-month post-treatment mark. Furthermore, compared to the TAU only group, adolescents in IERITA plus TAU group demonstrated significantly larger improvements in self-reported emotion dysregulation (1-month posttreatment p<0.01, 3-month posttreatment p=0.01), self-reported self-destructive behaviors (p<0.001, p<0.001), and assessor-rated global functioning (p=0.02, p=0.009) at both 1-and 3-month posttreatment. Mediation analysis revealed week-to-week improvements in emotion dysregulation mediated week-to-week reductions in NSSI frequency in IERITA. Overall, these findings support therapist-guided IERITA delivered adjunctive to TAU over 12 weeks as an effective treatment for NSSI, by targeting emotion dysregulation.
1. In preterm infants with respiratory distress, there was no difference in time to full enteral feeding (FEF), between the nasal continuous positive airway pressure (NCPAP) and heated humidified high-flow nasal cannula (HHHFNC) groups.
2. The NCPAP group had a lower rate of ineffectiveness than the HHHFNC in treating respiratory distress syndrome (RDS)
Evidence Rating Level: 1 (Evidence)
RDS is common in preterm infants, and noninvasive respiratory support (NRS) modalities like NCPAP and HHHFNC are employed to mitigate adverse events in these infants. While preterm infants benefit from early initiation of enteral feeding, many experience feeding intolerance. The pressurized gas flow, gaseous distension of the intestine, and the oxygen-enriched air mixture associated with NRS may affect feeding intolerance in preterm infants. Therefore, this multicenter randomized control trial aimed to compare the effects of NCPAP and HHHFNC on feeding intolerance in preterm infants with RDS. 247 infants (median [IQR] gestational age 28 [27-29] weeks, 52.6% female) born between November 2018 and June 2021, diagnosed with RDS, and who passed stability testing, were randomized to either HHHFNC (n=122) or NCPAP (n=125). The median time to reach FEF was 14 days (95% CI, 11-15 days) in the NCPAP group, which was not significantly different than 14 days (95% CI, 12-18 days) in the HHHFNC group at (p=0.85). Furthermore, between the two groups, there were no significant differences in secondary nutritional outcomes—no difference in weight growth, feeding interruption, feeding interruption lasting more than 24 hours, pathological gastric residual volume, frequent vomiting or regurgitation, and abdominal distension. Between randomization and time to reach FEF, 68.0% of infants in the NCPAP group and 60.8% in the HHHFNC group changed or discontinued their assigned NRS. The NCPAP group had a lower proportion of patients switching due to treatment ineffectiveness compared to the HHHFNC group (4.8% vs. 73.9%, p<0.001). Additionally, at the time of the first change, the NCPAP group showed a higher median SpO2–FIO2 ratio compared to the HHHFNC group (p < .001). Overall, this study found that feeding intolerance did not significantly differ between preterm infants in the NCPAP and HHHFNC groups, but some short-term respiratory outcomes were better with NCPAP.
Association between hyperlipidemia and trigger finger: A nationwide population-based cohort study
1. In a large Taiwanese cohort, it was found that patients with hyperlipidemia had higher risk of developing stenosing tenosynovitis, otherwise known as trigger finger, compared to controls.
Trigger finger, also referred to as stenosing tenosynovitis, is a common condition in those aged 50 to 60 years. The disease is characterized by pain and locking of fingers, particularly the thumb and fourth finger. The etiology of trigger finger is poorly understood, with female sex, obesity, carpal tunnel syndrome, and rheumatoid arthritis being reported as possible risk factors. National Health Insurance Research Database (NHIRD) in Taiwan was used to identify and evaluate a cohort of 41,421 patients with hyperlipidemia (mean age 49.49 years) and 82,842 controls (mean age 49.90 years) to investigate the association between hyperlipidemia and trigger finger. Baseline demographic characteristics, namely distribution of urbanization, distribution of insurance amounts, and comorbidities, significantly differed between the two groups. The incidence of trigger finger was 24.62 per 10,000 person-years in the hyperlipidemia cohort and 6.37 per 10,000 person-years in the control cohort. After adjusting for confounders, the hyperlipidemia cohort had a significantly higher adjusted HR for trigger finger (4.03; 95% CI, 3.57–4.55; P < 0.001) compared with the control. Sex stratification demonstrated trigger finger adjusted HRs of 4.59 (95% CI, 3.67–5.73; P < 0.001) for males and 3.77 (95% CI, 3.26–4.36; P < 0.001) for females in the hyperlipidemia cohort. Overall, this study demonstrates that individuals with hyperlipidemia are at an increased risk of developing trigger finger, even after accounting for disparities in comorbidities. Therefore, metabolic screening for patients with trigger finger could facilitate early detection and management of hyperlipidemia, which is often clinically silent for years.
Image: PD
©2023 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.