2 Minute Medicine Rewind July 20 – 26, 2015
Chemotherapy Use, Performance Status, and Quality of Life at the End of Life
While the administration of chemotherapy in end-stage cancer patients with good performance status may improve quality of life, it is unclear whether individuals nearing death confer the same benefit. The American Society of Clinical Oncology (ASCO) currently recommends palliative chemotherapy for patients with solid tumors only in individuals with good baseline performance status. In this multicenter prospective cohort study, 312 patients with end-stage cancer and a physician-estimated life expectancy of £6 months were followed until death to study the effect of chemotherapy on quality of life near death (QOD) as a function of baseline performance status. Performance status was measured using the respective Eastern Cooperative Oncology Group (ECOG) scale. Postmortem interviews with caregivers were used to assess QOD based on the patient’s final week of life. Consistent with ASCO guidelines, patients that received chemotherapy at study enrollment had better performance status scores compared to patients that did not receive chemotherapy (ECOG 1.6 vs. 2.0, p<0.001). Researchers found that upon adjusting for baseline performance status and study enrollment site, patients’ risk of death was not associated with chemotherapy use (HR: 0.85, 95% CI 0.65-1.11). However, in examining the relationship between chemotherapy use and QOD, the authors found that in patients with good baseline performance status, QOD was decreased in those that received palliative chemotherapy (OR 0.35, 95% CI 0.17-0.75; RR 0.64, 95% CI 0.46-0.88). The receipt of palliative chemotherapy in patients with moderate or poor baseline performance status did not appear to impact QOD.
This study therefore shows that the patients most likely to receive palliative chemotherapy (ECOG performance status £1) had significantly poorer QOD compared to those who did not receive chemotherapy. With no observable survival benefit in patients that received chemotherapy, this study suggests that palliative chemotherapy for patients with end-stage cancer nearing death may be of limited clinical value.
Long-Term Outcomes of Abdominal Aortic Aneurysm in the Medicare Population
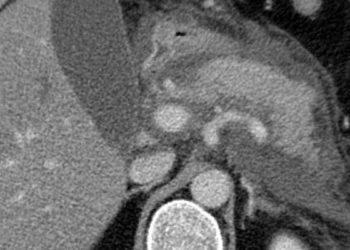
Compared with open repair of abdominal aortic aneurysm, endovascular repair is associated with lower perioperative morbidity and mortality. Whether endovascular repair confers greater long-term survival, however, is unclear. In a previous study using Medicare data that accounted for over 83% of abdominal aortic aneurysm repairs in the United States, the authors found that at 4-year follow-up, an increased rate of aneurysm-related reintervention in the endovascular repair group was balanced in the open repair group by an increased rate of reintervention for laparotomy-related complications. In this retrospective cohort study, investigators studied perioperative and long-term survival, reinterventions and complications in propensity-score-matched cohorts (39,966 patients per cohort) of Medicare beneficiaries that had undergone either endovascular or open repair for abdominal aortic aneurysm, forming a total study population of 79,932 patients.
Researchers found that perioperative mortality, defined as death during the index admission or within 30 days after surgery, was increased in patients that received open repair compared to the endovascular repair group (RR 3.22, 95% CI 2.95-3.51). In assessing long-term survival, the investigators found that patients who received endovascular repair gained an early survival benefit for approximately 3 years, after which survival rates were similar between the cohorts. Further analysis of survival rates revealed that the endovascular technique was markedly superior to open repair at 30 days (HR 0.32, 95% CI 0.29-0.35) and 90 days postoperatively (HR 0.64, 95% CI 0.58-0.71). With respect to other long-term outcomes, the authors found that at 8 years of follow-up, aneurysm rupture occurred more frequently in the endovascular repair group at 5.4% compared to the open repair group at 1.4% (p<0.001). At this time, aneurysm-related interventions were also more common in the endovascular repair cohort (18.8% vs. 3.7%, p<0.001). Consistent with previous studies, reinterventions for laparotomy-related complications were more common in the open repair group (17.7% vs. 8.2%, p<0.001). Overall rates of intervention for aneurysm- and laparotomy-related complications were 25.1% in the endovascular repair group versus 20.6% in the open-repair group. This study therefore shows that patients who undergo endovascular repair for abdominal aortic aneurysm confer an early survival advantage compared to those that undergo open repair. It should be noted, however, that complications related to late rupture are significantly higher among patients who receive endovascular repair.
In addition to certain lifestyle and genetic factors, early life development has been associated with the risk of developing type 2 diabetes in later life. Prior studies have indicated associations between low birth weight and the risk of developing type 2 diabetes in overweight adults. Few studies, however, have examined potential interactions between prenatal and postnatal factors. Using detailed information on lifestyle habits and medical history from the Health Professionals Follow-up Study, Nurses’ Health Study and Nurses’ Health Study II, this prospective cohort study of 149,794 patients assessed the joint association of birth weight and established lifestyle risk factors with incident type 2 diabetes. All patients were free of cardiovascular disease, cancer and diabetes at baseline.Over the course of 20-30 years of follow-up,11,709 incident cases of type 2 diabetes were identified. Researchers found that across all cohorts from the aforementioned databases, there was a consistent association between low birth weight and risk of type 2 diabetes. Compared to people with a birth weight of 3.18-3.82 kg, those falling within the lowest birth weight category of <2.5 kg had an elevated risk of type 2 diabetes (RR 1.49, 95% CI 1.39-1.60). This risk was amplified upon further adjustment for current body mass index (BMI) (RR 1.55, 95% CI 1.46-1.64). In a more in-depth analysis, study participants were classified according to joint categories of birth weight and an unhealthy lifestyle score based on diet, smoking status, physical activity, alcohol consumption and BMI. An increased risk of type 2 diabetes was found per unhealthy lifestyle factor (RR 2.10, 95% CI 2.26-3.63) and per kg lowering of birth weight (RR 1.45, 95% CI 1.32-1.59), with an excess risk due to interaction (RR 0.31, 95% CI 0.16-0.47). This study therefore shows that low birth weight and unhealthy lifestyle are significantly associated with an increased risk type 2 diabetes, with an interaction between the risk factors that exceeds the risk that would be conferred by the presence of each factor.
The receipt of neoadjuvant chemoradiotherapy in addition to surgery (NCRS) improves survival in patients with esophageal cancer compared to surgery alone. While National Comprehensive Cancer Network (NCCN) guidelines indicate that definitive chemoradiotherapy (dCRT) without surgery is a viable alternative to surgical resection for locally advanced squamous cell carcinoma, select patients with recurrent or persistent disease go on to be considered for salvage esophagectomy (SALV). The receipt of dCRT, however, has been associated with poor clinical outcomes in patients that subsequently undergo SALV. In this retrospective cohort study, 848 patients with esophageal cancer that received either SALV or NCRS with curative intent were compared to assess the impact of SALV on clinical outcomes. Researchers found that in-hospital mortality and morbidity were similar between SALV and NCRS groups, however anastomotic leaks (OR 1.732, 95% CI 1.110-2.703) and surgical site infections (OR 1.614, 95% CI 1.058-2.461) were increased in the SALV group. A subset analysis of the SALV group also revealed significantly greater in-hospital mortality (27.8% vs. 4.3%, p<0.001), morbidity (75.9% vs. 61%, p=0.039), anastomotic leak (27.8% vs. 15%, p=0.023), surgical site infection and pulmonary complications (55.6% vs. 40.2%, p=0.038) among patients who received a total radiation dose ³ 55 Gy, compared to patients that received < 55 Gy.This study therefore shows that SALV may in fact offer acceptable short- and long-term clinical outcomes after appropriate patient selection, taking into account treatment-related factors such as total radiation dose received.
Association of Child Poverty, Brain Development, and Academic Achievement
Children from lower socioeconomic groups perform poorer in standardized tests of academic achievement, have lower grades and educational attainment. These patterns continue into adulthood, ultimately contributing to socioeconomic disparities that have a direct impact on an individual’s overall health. In this prospective cohort study, the magnetic resonance imaging (MRI) scans of 389 children and adolescents from the National Institutes of Health Magnetic Resonance Imaging Study of Normal Brain Development were reviewed to determine whether atypical patterns of structural brain development underlie the relationship between low-income and reduced academic performance. Researchers found that children from low-income families had systematic structural differences in the frontal and temporal lobes, as well as the hippocampus. Regional gray matter volumes of children from households 1.5 times below the federal poverty level (FPL) were approximately 3-4% lower than developmental norms (p<0.05). In analyzing the relationship between brain development and academic achievement, researchers found that normal structural development of gray matter in areas that had atypical development has been seen in low-income children, was correlated with improved performance on tests of achievement. Mediation analyses indicate that developmental differences in frontal and temporal lobes may account for up to 15-20% of deficits in academic achievement among low-income children. This study therefore shows that certain atypical patterns of structural brain development may mediate the relationship between household poverty and poorer academic performance.
©2015 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.