2 Minute Medicine Rewind July 27 – August 3, 2014
In this section, we highlight the key high-impact studies, updates, and analyses published in medicine during the past week.
Spread of Artemisinin Resistance in Plasmodium falciparum Malaria
Since 2005, the World Health Organization has recommended the use of artemisinin-based combination therapies as the first line treatment for P. falciparum malaria in endemic areas due to resistance in these areas to other antimalarial drugs such as chloroquine and sulfadoxine-pyrimethamine. More recently, artemisinin resistance, characterized by slow parasite clearance in peripheral blood, has been observed and linked to point mutations in the propeller region of a P. falciparum “kelch” protein. The existence of artemisinin resistance was first noted in Cambodia, and this study aimed to map patterns and severity of resistance in different susceptible regions. In this open-label, randomized trial at 15 sites in 10 countries (Cambodia, Thailand, Laos, Vietnam, Myanmar, Bangladesh, India, Nigeria, Kenya and Democratic Republic of Congo), 1241 adults and children with uncomplicated P. falciparum malaria were enrolled between May 2011 and April 2013 to receive oral artesunate for 3 days followed by a standard 3 day course of artemisinin combination therapy, and the parasite clearance half lives in different regions were determined. Although the treatment course with a 6 day antimalarial therapy was associated with a 97.7% cure rate, slow clearing infections, defined by parasite clearance half life > 5hours, were detected throughout mainland Southeast Asia from southern Vietnam to central Maynmar. Median parasite clearance half lives ranged from 2 hours in Laos to 7 hours in Thailand. Incidence of pre and post treatment gametocytemia, a marker for transmission, was also higher in patients with longer parasite clearance half life. Thus, despite the recent successes in antimalarial therapies, future gains in the malaria treatment might be limited with the spread of artemisinin resistance and emergence of resistance to unprotected partner drugs in artemisinin combination regimens.
Spiroindolone KAE609 for Plasmodium falciparum and Plasmodium vivax Malaria
With the rise of artemisinin resistance in P. falciparum, the search for alternative treatment regiments became important. This phase 2 trial conducted in three centers in Thailand examined the efficacy of spiroindolone antimalarial agent KAE609 in the treatment of falciparum and vivax malaria. KAE609 is a first in its class agent targeting parasite plasma membrane Na+-ATPase that regulates sodium and osmotic homeostasis. Ten P. vivax and eleven P. falciparum uncomplicated malaria patients were enrolled in the trial and treated with KAE609 at an oral dose of 30 mg per day for 3 days, with the parasite clearance rate studied as the primary endpoint. The median parasite clearance half life after the administration of KAE609 in the P. falciparum cohort was 0.90 hours (interquartile range, 0.78 to 1.07), and it was 0.95 hours (interquartile range, 0.85 to 1.14) in the P. vivax group. The study was too small to derive any valid conclusions regarding the safety of KAE609, but no significant side effects leading to discontinuation of the drug were observed in the trial, with nausea as the most reported adverse event. This study thus showed that spiroindolone KAE609 might be an important antimalarial drug with rapid activity against P. falciparum and P. vivax, with further studies needed for its safety determination.
Pregnancy Incidence and Outcomes Among Women Receiving Preexposure Prophylaxis for HIV Prevention
Daily tenofovirdisoproxilfumarate (TDF) or emtricitabine/tenofovirdisoproxilfumarate (FTC/TDF) have been shown to be effective as antiretroviral preexposure prophylaxis in HIV serodiscordant couples. Based on animal experiments and observational human studies, both TDF and FTC are labeled as pregnancy category B drugs; however, no randomized placebo controlled trials have been conducted to date to investigate pregnancy outcomes in women taking antiretroviral preexposure prophylaxis. In this randomized trial, 1785 HIV uninfected females with serodiscordant partners in Uganda and Kenya were assigned to daily oral FTC/TDF therapy (n = 566), TDF alone (598), or placebo groups (621), with placebo group discontinued when preexposure prophylaxis was determined to be efficacious in prevention of HIV transmission in 2011. Pregnancy incidence, birth outcomes, and infant growth were studied in the three groups. Of note, study medications were only continued until conception in this trial. Pregnancy incidence was observed to be 10 per 100 person years in the placebo group, as compared to 8.8 in FTC/TDF group (difference from placebo -1.3; 95% CI -4.1 to 1.5; p=0.39), and 11.9 in TDF group (difference from placebo 1.9; 95% CI -1.1 to 4.9; p=0.22). Pregnancy loss was 32.3% in placebo group, as compared to 42.5% in FTC+TDF group (difference from placebo 10.2%; 95% CI -5.3% to 25.7%; p=0.16) and 27.7% in TDF group (difference from placebo -4.6%; 95% CI -18.1% to 8.9%; p=0.46). The rates of preterm birth, congenital anomalies, and growth abnormalities within the first year of life did not differ significantly among groups. This study thus showed that pregnancy incidence and birth outcomes are not statistically different for women receiving preexposure HIV prophylaxis compared to placebo; however, given wide confidence intervals and discontinuation of prophylaxis at conception, further studies are needed to definitively understand the safety of preexposure prophylaxis in pregnancy.
HCV genotype 1 infections have previously been treated with peglyated interferon-alpfa, ribavirin, and an addition of HCV NS3/4A protease inhibitor boceprevir or telaprevir due to poor treatment response to peglyated interferon-alpfa and ribavirin alone. However, treatment with the addition of a protease inhibitor was limited by high rates of severe adverse events as well as high pill burden contributing to noncompliance. Simeprevir is another protease inhibitor that has a once daily dosing and has been shown in phase 2a and 2b trials to have a favorable efficacy and safety profiles in the treatment of HCV genotype 1 infections. In this phase 3, randomized, double blind multicenter trial, 394 patients with chronic HCV genotype 1 infection and no prior HCV treatment were randomized in a 2:1 ratio to receive simeprevir plus peginterferon plus ribavirin for 12 weeks, followed by peginterferon plus ribavirin (simeprevir group), or placebo plus peginterferon plus ribavirin for 12 weeks, followed by peginterferon plus ribavirin (placebo group) to study the effect of treatment on sustained virological response 12 weeks after the planned end of treatment course. Sustained virological response at 12 weeks was achieved in a higher percentage of patients in simeprevir group (80%) compared to placebo group (50%), with difference stratified by HCV genotype 1 subtype and IL28B genotype significant at 29.3%; 95% CI 20.1-38.6; p<0.001. Overall rates of adverse effects were similar in the two groups during the entire treatment course. The study thus concluded that simeprevir plus peginterferonalfa 1a plus ribavirin has superior efficacy compared to peginterferon plus ribavirin alone in the treatment of naïve patients with HCV genotype 1 infection.
In 2011, UN General Assembly has adopted an agreement that committed its member states to adopt nine global targets to reduce the premature mortality from four main non-communicable diseases, including cardiovascular diseases, chronic respiratory diseases, cancers and diabetes, by 25% from 2010 to 2025 (termed 25×25 target). Premature mortality was defined as probability of dying from noncommunicable diseases between ages 30 and 70 years of age in the absence of other competing causes. This study then aimed at estimating the impact of achieving only six risk factor targets (tobacco smoking, alcohol use, salt intake, obesity, raised blood pressure and glucose) in reducing the premature mortality and reaching the 25×25 target. The analyses showed that without any interventions, based on projections taking into account the current trends, the probability of premature mortality from noncommunicable diseases is expected to decrease between 2010 and 2025 on the global scale by an estimated 11% for men and 10% for women, with the largest contribution from decreased mortality from cardiovascular and chronic respiratory diseases. Despite the decrease in percent mortality, absolute number of deaths is expected to rise due to population growth as well as an increase in the aging population. According to the study’s estimates, achieving the six risk factor targets is expected to lead to a total reduction in premature mortality from non-communicable diseases of 22% in men and 19% in women – which is equivalent to 5.6 million fewer worldwide deaths from non-communicable disease in 2025 compared to the number of deaths if risk factor targets are not met. Achieving the risk factor targets is expected to lead to greater than 25% decrease in premature deaths from ischemic heart disease, stroke, hypertensive heart disease and COPD. Lung and stomach cancer deaths are expected to be reduced by 12-19%. Mortality from diabetes, breast, cervical and colorectal cancers are only projected to be reduced by small amounts by meeting the risk factor targets. Risk factor goals expected to lead to the greatest reduction in mortality are projected to be blood pressure and tobacco use. Importantly, the largest influence on non-communicable disease mortality by meeting the risk factor targets is expected to be seen in low to middle income countries. Therefore, based on the results of this study, reaching just six risk factor targets would not completely allow us to achieve the 25×25 goal; however, it will close 77% of the gap between the current trends and the set goal, with the largest expected effect in the low to middle income countries.
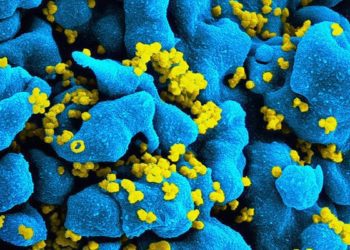
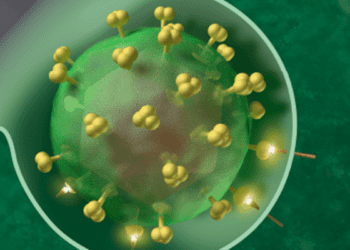
Image: PD
©2012-2014 2minutemedicine.com. All rights reserved. No works may be reproduced without written consent from 2minutemedicine.com. Disclaimer: We present factual information directly from peer reviewed medical journals. No post should be construed as medical advice and is not intended as such by the authors or by 2minutemedicine.com. PLEASE SEE A HEALTHCARE PROVIDER IN YOUR AREA IF YOU SEEK MEDICAL ADVICE OF ANY SORT.