2 Minute Medicine Rewind July 31, 2017
Ventilation in Extremely Preterm Infants and Respiratory Function at 8 Years
Infants born prior to 28 weeks of gestation, or extremely preterm, often require assisted ventilation to allow enough time for their lungs to mature. In this retrospective cohort study, extremely preterm infants born during three time periods (1991-1992, 1997, 2005) were followed up to investigate the short- and long-term effects of assisted ventilation and oxygen therapy on lung function at 36 weeks and 8 years. Researchers found that the duration of assisted ventilation increased over time with a mean time of 53.2 days in the 2005 group and a mean time of 33.3 days in the 1991 and 1992 group (p<0.05). Over time, less invasive nasal continuous positive airway pressure (CPAP) was also utilized more, as it was used for a mean of 33.3 days in the 2005 subset, as compared to 26 days in the 1997 subset (p<0.05) and 8.9 days in the 1991 and 1992 subset (p<0.05). However, the rate of oxygen dependence at 36 weeks increased in the 2005 cohort with 56% of infants still requiring oxygen as compared to 43% of infants in the 1997 cohort (p<0.05). Additionally, the forced expiratory volume in one second to forced vital capacity ratio (FEV1/FVC) had a mean difference in z scores of -0.75 (95% CI -1.07 to -0.44, p<0.001) when comparing the 2005 cohort to the 1991 and 1992 cohort and had a mean difference in z scores of -0.53 (95% CI -0.86 to -0.19, p=0.002) when comparing the 2005 group to the 1997 group. This study therefore shows that increased use of less invasive ventilation methods was not associated with less oxygen dependence at 36 weeks or improved lung function at 8 years.
There is debate surrounding the role of electronic cigarettes (e-cigarettes) in smoking cessation. In this study, the authors examined whether recent increased use of e-cigarettes has been associated with a change in overall rates of smoking cessation (quitting for at least 3 months) at the population level, based on data from the US Current Population Survey-Tobacco Use Supplement (CPS-TUS) for the years 2001-2002, 2003, 2006-2007, 2010-2011, and 2014-15. Researchers found that the rate of smoking cessation was significantly higher in 2014-2015 than in 2010-2011, yielding a 1.1% increase in smoking cessation rate (95% CI 0.6% to 1.5%). The smoking cessation rate was also significantly higher in 2014-2015 than in all other previous years that data was collected for. Additionally, in 2014-2015, 38.2% of current smokers and 49.3% of recent quitters had tried e-cigarettes while 11.5% of current smokers and 19% of recent quitters used e-cigarettes currently. It was found that e-cigarette users were more likely than non-users to attempt to quit smoking, as the rate of attempted quitting was 25.0% higher in those using e-cigarettes (95% CI 23.2% to 26.9%). E-cigarette users were also more likely to succeed in quitting, with a 3.5% increase in success rate (95% CI 2.5 to 4.5%). Investigators therefore concluded that the increase in e-cigarette use was associated with an increase in smoking cessation at the population level.
Vascular endothelial growth factor (VEGF) is an important target in slowing and/or stopping tumor angiogenesis, an important step in the progression of cervical cancer. This randomized, controlled, phase 3 trial investigated the effects of bevacizumab, an anti-VEGF monoclonal antibody, in those with persistent, recurrent, or metastatic cervical cancer on overall survival. From 2009 to 2012, 452 patients were randomly assigned to one of four groups, receiving IV chemotherapy with cisplatin and paclitaxel alone, or with bevacizumab, or receiving topotecan and paclitaxel alone, or with bevacizumab. These therapies were given in 21-day cycles until one of the following endpoints: complete response, unacceptable toxicity, disease progression, or withdrawal from the study by the patient. Results showed that the two groups who received bevacizumab had improved survival compared to those who received chemotherapy alone (16.8 months vs.13.3 months HR 0.77, 95% CI 0.62 to 0.95, p=0.007). Postprogession overall survival, however, was not significantly different between the two groups (p=0.06). This study therefore shows that bevacizumab therapy may result in increases in overall survival.
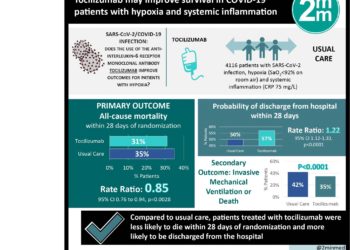
Trial of Tocilizumab in Giant-Cell Arteritis
Glucocorticoids are frequently used in the treatment of giant-cell arteritis (GCA). However, when they are used long-term they may cause significant side effects. In this randomized controlled trial, tocilizumab, a monoclonal antibody directed against the interleukin-6 receptor alpha, was investigated for its use in preventing relapse as glucocorticoids are tapered. Patients were randomly assigned to four treatment groups, receiving subcutaneous tocilizumab every week or every other week along with a 26-week prednisone taper or receiving placebo with a 26-week prednisone taper or a 52-week prednisone taper. Researchers found that the primary outcome of glucocorticoid-free remission at 52 weeks was significantly increased in those treated with tocilizumab, occurring in 56% of patients treated with tocilizumab every week, 53% of patients who received tocilizumab every other week, 14% of those who received placebo with a 26-week taper and 18% of those who received placebo with a 52-week taper (p<0.001 when comparing either tocilizumab group to either placebo group). The cumulative prednisone dose was also significantly decreased for the arms treated with tocilizumab, as compared to the placebo arms of the study (p<0.001). It was also found that while 15% of those receiving tocilizumab every week and 14% of those receiving it every other week had adverse events, 25% of those in the placebo with 52-week taper group and 22% of those in the placebo with 26-week taper group had adverse events. It was concluded that tocilizumab with a glucocorticoid taper was more efficacious in achieving glucocorticoid-free remission in patients with GCA, as compared to placebo with a glucocorticoid taper.
Currently, the standard duration for targeted temperature management (TTM) at 33°C to 36°C in patients with out-of-hospital cardiac arrest is 24 hours. This randomized controlled trial sought to investigate whether 48 hours of TTM was superior to standard 24-hour TTM with respect to neurologic outcomes. As part of this multicenter trial, 355 patients were enrolled from 2013 to 2016 and assigned to receive either 48 hours of TTM or 24 hours of TTM. The patients were then followed up for an endpoint of favorable neurologic outcome at 6 months as indicated by a Cerebral Performance Categories (CPC) score of 1 or 2. It was found that 48 hours of TTM did not result in a statistically significant increase in favorable outcome, as 69% had a CPC score of 1 or 2 in that group, as compared to 64% in the 24-hour group (RR 1.08, 95% CI 0.93 to 1.25, p=0.33). Mortality at six months also did not differ significantly between the two groups (RR 0.81, 95% CI 0.59 to 1.11, p=0.19). Adverse events, however, were more likely to occur in the 48-hour TTM group (RR 1.06, 95% CI 1.01 to 1.12, p=0.03). This study therefore shows that in unconscious survivors from out-of-hospital cardiac arrest, TTM for 48 hours did not significantly improve 6-month neurologic outcomes as compared to standard 24-hour TTM.
Image: PD
©2017 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.

![The ABCD2 score: Risk of stroke after Transient Ischemic Attack (TIA) [Classics Series]](https://www.2minutemedicine.com/wp-content/uploads/2013/05/web-cover-classics-with-logo-medicine-BW-small-jpg-350x250.jpg)