2 Minute Medicine Rewind July 8 – July 15, 2014
In this section, we highlight the key high-impact studies, updates, and analyses published in medicine during the past week.
Letrozole versus Clomiphene for Infertility in the Polycystic Ovary Syndrome
Polycystic ovary syndrome (PCOS) affects 5 to 10 percent of reproductive age women and is the major cause of anovulatory infertility. Clomiphene, a selective estrogen receptor modulator, is currently the first-line treatment for infertility in women with PCOS. However, a relatively poor efficacy and poor side effect profile has been observed with clomiphene, necessitating a search for an alternative treatment for infertility. In this study, letrozole, an aromatase inhibitor, was investigated as an alternative infertility therapy in PCOS. In this double-blind multicenter trial, 750 infertile women ages 18 – 40 with PCOS were randomly assigned to received clomiphene or letrozole for up to five treatment cycles to study the effect of the drug on success of pregnancies and pregnancy outcomes. Study found that ovulation (834 of 1352 treatments vs 688 of 1425 treatments , p<0.001) and live births (103 of 374 vs 72 of 376, p=0.007) were higher in women in letrozole compared to clomiphene groups. The rate of pregnancy loss (49 of 154 in letrozole group vs 30 of 103 in clomiphene group) did not differ significantly between treatment groups. Similarly, mean pregnancy duration, birth weight, and rates of neonatal complications were similar, although more neonatal anomalies were observed in letrozole compared to clomiphene group (4 anomalies in letrozole group vs 1 anomaly in clomiphene group, p = 0.65), with difference in the number of anomalies not statistically significant. The study therefore shows that letrozole is possibly a more effective fertility treatment compared to clomiphene for women with PCOS.
Approximately 150,000 cholecystectomies due to calculous cholecystitis are done each year in the United States, and although the role of pre-operative and intra-operative antibiotics in preventing infections is known in this condition, there is no clear data guiding the necessity of post-operative antibiotics. In this open label, parallel group, randomized control multicenter trial, 414 patients with grade I or II acute calculous cholecystitis who received pre and intra-operative Augmentin were randomized to receive either post-op Augmentin 3 times daily for five days or no antibiotic therapy in order to determine whether post-operative antibiotics are useful in preventing surgical site and distant infections within a 4 week post-operative period. A total of 66 patients in this trial developed postoperative infections within a 4 week post-surgical period, with 35 patients in the no antibiotic group and 31 patients in the Augmentin group developing infections. In imputed intention to treat analysis of 414 patients, infection rates were 17% in the non-treatment group and 15% in the antibiotic group, with absolute difference 1.93% (95% CI of -8.98% to 5.12%). Clavien complication severity outcomes were comparable in both Augmentin and no antibiotic groups. Bile cultures, collected from 93% of patients involved in the trial, showed sterile cultures in 60.9% of cases. This study therefore shows that post-operative Augmentin might not be necessary in the post-operative period as it does not reduce the incidence of postoperative infections in cholecystectomies performed for mild to moderate calculous cholecystitis.
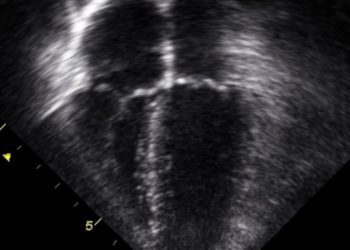
Effects of Hypothermia for Perinatal Asphyxia on Childhood Outcomes
Perinatal asphyxial encephalopathy is associated with high mortality and neurodevelopmental impairment, and one potential early intervention available for this condition is induced hypothermia for 72 hours initiated within 6 hours of delivery. Although studies have shown reduced risks of neurological impairments at 18 months of age in children who underwent induced hypothermia at birth, there is no clear evidence to suggest whether such therapy offers longer term neurocognitive benefits. In this randomized control trial, 325 newborns with asphyxial encephalopathy who were born at 36 weeks or greater were randomized to receive standard post-natal care alone or standard post-natal care combined with hypothermia induction to study the effect of hypothermia on survival with an IQ score of 85 or higher. 52% of children in the hypothermia group versus 39% of children in the standard treatment group survived with an IQ score at 85 or above; relative risk was calculated to be 1.31, with p=0.04. Interestingly, the mortality rates in hypothermia and control groups were similar; however, 45% of children in the hypothermia group survived without major neurological abnormalities as compared to 28% of children within the control group, with relative risk of 1.60 (95% confidence interval of 1.15 to 2.22). Thus, this study shows that although hypothermia as treatment for perinatal asphyxia does not decrease mortality, it does improve neurocognitive outcomes, with significant reductions in cerebral palsy and moderate to severe disability.
Encouraging and supporting smoking cessation efforts is an important goal for the healthcare professionals, and currently a number of therapies are available to help active smokers in their efforts to quit. These therapies include nicotine replacement products as well as varenicline; however, studies to date have not determined the efficacy of combination therapy with varenicline and nicotine replacement therapy. In this randomized, double-blinded, placebo-controlled clinical trial conducted in 7 centers in South Africa, 446 otherwise healthy smokers were randomized to nicotine replacement plus varenicline vs. placebo plus varenicline treatment groups to evaluate the effects of these therapies on smoking cessation as determined by exhaled carbon monoxide measurements at target quit date and up to 24 weeks following that date. Nicotine replacement therapy was started 2 weeks prior to a target quit date and continued for 12 weeks. Varenicline was started 1 week prior to target quit date and continued for 12 weeks. The combination of nicotine replacement therapy and varenicline was associated with a higher continuous abstinence rate at 12 and 24 weeks as compared to varenicline therapy alone. Therefore, this study demonstrates that varenicline and nicotine replacement in combination offer a superior treatment regiment compared to varenicline alone, at least in the short term following initiation of therapy. There is no evidence to date on the longer term effects of these therapies for smoking cessation.
Image: PD
©2012-2014 2minutemedicine.com. All rights reserved. No works may be reproduced without written consent from 2minutemedicine.com. Disclaimer: We present factual information directly from peer reviewed medical journals. No post should be construed as medical advice and is not intended as such by the authors or by 2minutemedicine.com. PLEASE SEE A HEALTHCARE PROVIDER IN YOUR AREA IF YOU SEEK MEDICAL ADVICE OF ANY SORT.





![Improved hematologic cancer survival in Europe over a 15 year period [EUROCARE-5 study]](https://www.2minutemedicine.com/wp-content/uploads/2014/07/700px-Europe_polar_stereographic_Caucasus_Urals_boundary.svg_-75x75.png)
