2 Minute Medicine Rewind June 1, 2020
1. In patients with confirmed SARS-CoV-2 infection within 7 days before or 30 days after surgery, significant mortality was observed, and perioperative pulmonary complications occurred in more than half the patients.
Evidence Rating: 2 (Good)
Current guidelines regarding the management of surgical patients during the SARS-CoV-2 pandemic are based solely on expert opinion rather than systematic investigation. With spread to the majority of countries worldwide and significant burden in North America, the impact of the pandemic on postoperative recovery and outcomes must be meaningfully sorted out to better inform clinical decision making in these unprecedented times. To address this knowledge gap, investigators performed an international multicentre cohort study with 1128 surgical patients at 235 hospitals in 24 different countries. Of the 1128 patients included, 835 had received emergency surgery and 280 had received elective surgery. Positive infection was identified preoperatively in 294 patients and postoperatively in 806, either by quantitative RT-PCR or a combination of radiological and clinical findings. Primary outcome was 30-day postoperative mortality, and the secondary outcome measure of interest was pulmonary complications, consisting of pneumonia, ARDS, or unexpected postoperative ventilation. Thirty day mortality rates were observed to be 23.8%, much higher than the pre-established baseline of 3% from prior investigations. A significant portion of these deaths were due to pulmonary complications (82.6%), which were present in 51.2% of SARS-CoV-2 positive patients. Again, this is much higher than the 10% that has previously been identified as the baseline rate of perioperative pulmonary complications. In adjusted analyses, male sex (odds ratio 1·75 [95% CI 1·28–2·40], p<0·0001), age 70 years or older versus younger than 70 years (2·30 [1·65–3·22], p<0·0001), concurrent morbidities (as identified as American Society of Anesthesiologists grades 3–5 versus grades 1–2) (2·35 [1·57–3·53], p<0·0001), malignant versus benign or obstetric diagnosis (1·55 [1·01–2·39], p=0·046), emergency versus elective surgery (1·67 [1·06–2·63], p=0·026), and major versus minor surgery (1·52 [1·01–2·31], p=0·047) were identified as factors associated with 30-day mortality. Although not all patients were identified as SARS-CoV-2 positive via laboratory investigation, study findings strongly suggest that perioperative infection with SARS-CoV-2 is associated with high rates of mortality and pulmonary complications relative to pre-established observations. As such, clinicians are advised by investigators to have a higher threshold for surgical intervention, and take additional measures in preventing infection in preventing infection in surgical patients if possible.
Comparison of 3 Treatment Strategies for Medication Overuse Headache
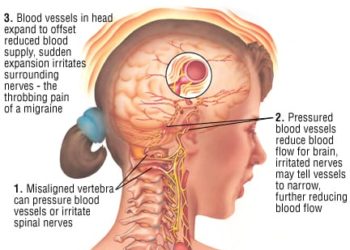
1. For patients with medication overuse headache, withdrawal and preventive medication was more effective at reducing headache than other strategy alone.
Evidence Rating: 1 (Excellent)
Medication overuse headache (MOH) affects more than 60 million people globally and is considerably disabling. Although current guidelines recommend withdrawal of medication and preventive medication usage, there is currently great debate regarding what the most effective strategy is for treating the condition. In this open-label, randomized clinical trial, researchers enrolled 120 patients with MOH to determine whether preventive medication alone, withdrawal alone, or a combination of the two would be the most effective treatment strategy. The withdrawal group would receive withdrawal advice and MOH education from trained headache nurses, followed by complete discontinuation of analgesics for 2 months, though rescue medications and antiemetics could be used during the treatment period. Preventive medication varied depending on the presenting complaint, and was adherent to guidelines outlined according to the Danish Headache Centre. Primary outcome was change in headache (days per month) from baseline at 6 months. Several secondary outcomes were also included, such as reduction of migraine days per month, reversion to episodic headaches, use of short-term medication, headache intensity, and number of patients with medication overuse at 6 months, for example. Headache days per month were most greatly reduced in the withdrawal plus preventive group (12.3; 95% CI, 9.3-15.3), by 9.9 (95% CI, 7.2-12.6) in the preventive group, and by 8.5 (95% CI, 5.6-11.5) in the withdrawal group (P = .20). Although no differences were found in reduction of migraine days per month or headache intensity, 23 of 31 patients (74.2%) in the combination therapy group reverted to episodic headache, compared with 21 of 35 (60.0%) in the preventive group and 15 of 36 (41.7%) in the withdrawal group (P = .03). Likewise, 30 of 31 patients (96.8%) in the withdrawal plus preventive group were cured of MOH, compared with 26 of 35 (74.3%) in the preventive group and 32 of 36 (88.9%) in the withdrawal group (P = .03), corresponding to a 30% (relative risk, 1.3; 95% CI, 1.1-1.6) increased chance of MOH cure in the combinational therapy group compared with the preventive group (P = .03). While findings suggest that all three treatment strategies were effective in reducing MOH, combinational therapy with withdrawal and preventive medication appears to be the superior method. The study primarily consisted of patients with MOH secondary to simple analgesic overuse however, and as such, further large scale RCT’s should be performed to improve generalizability of findings and better inform clinical decision making for MOH treatment.
Bariatric Surgery and Long-term Survival in Patients With Obesity and End-stage Kidney Disease
1. Bariatric surgery for patients with obesity and end-stage kidney disease was associated with lower all-cause mortality at 5 years.
Evidence Rating: 2 (Good)
Obesity and end-stage kidney disease are significant causes of mortality and morbidity in North America, and represents a significant burden to the healthcare system. Bariatric Surgery has been associated with lower risks of hyperglycaemia, hypertension, and adverse cardiovascular events in patients with obesity and type 2 diabetes. In patients with end-stage renal disease (ESRD) however, bariatric surgery rates remain low due to speculation of surgical complications and lack of literature demonstrating a clear benefit. To further investigate the benefits or harms of bariatric surgery for obese ESRD patients, researchers conducted a retrospective cohort study with data from the United States Renal Data System registry. Specifically, Cox proportional hazards analysis was used to evaluate differences in long-term survival among 1597 surgical and a matched cohort of 4750 nonsurgical patients with ESRD and obesity. Bariatric surgery was associated with lower all-cause mortality at 5 years compared with standard care (cumulative incidence, 25.6% vs. 39.8%; hazard ratio, 0.69, 95% CI, 0.60-0.78), primarily driven by lower rates of cardiovascular causes (cumulative incidence, 8.4% vs. 17.2%; hazard ratio, 0.51; 95% CI, 0.41-0.65). Interestingly however, bariatric surgery was associated with higher all-cause mortality at one year (cumulative incidence, 8.6% vs. 7.7%; hazard ratio, 1.45; 95% CI, 1.13-1.85), and increase in kidney transplant at 5 years (cumulative incidence, 33.0% vs. 20.4%; adjusted hazard ratio, 1.82; 95% CI, 1.58-2.09). This population-based study of patients with obesity and ESRD found a long term mortality benefit associated with bariatric surgery. Although further investigations need to be carried out to better meaningfully sort out the possible health benefits of bariatric surgery, findings suggest that the health benefits of surgery for patients with obesity can be generalized with patients with concomitant ESRD.
Description of COVID-19 in HIV-infected individuals: a single-centre, prospective cohort
1. Clinical characteristics of HIV-infected individuals appear to be similar to that of the general population and as such should have a similar treatment approach applied.
Evidence Rating: 2 (Good)
Despite there being a significant population of infected individuals, the relationship between HIV and COVID-19 was poorly characterized. Specifically, it was unclear as to whether HIV-infected individuals may have been at increased risk of SARS-CoV-2 infection or severe disease, owing to lower CD4 cell counts or unsuppressed HIV viral load, or alternatively have reduced risk and variable clinical presentation from immunosuppression and regular antiviral therapy. In this observational prospective study, researchers followed up on the data of 2873 HIV-infected individuals, 51 of which whom were diagnosed with COVID-19 (35 laboratory confirmed, 16 suspected). Thirty eight (75%) patients had mild or moderate disease, six (12%) individuals were critically ill, and two (4%) died. When comparing HIV positive patients with and without SARS-CoV-2 infection, no differences were found in the age distribution, nadir CD4 cell counts, and the proportion of individuals on ART, though patients with COVID-19 had a higher median body-mass index and prevalence of chronic comorbidities. Interestingly, a significantly higher proportion of COVID-19 infected patients had received tenofovir before COVID-19 diagnosis compared to SARS-CoV-2 negative patients (73% versus 38%). Lymphocyte counts were correlated with CD4 counts (ρ=0·54; p=0·0036), and individuals with lower lymphocytes counts were at higher risk of severe disease ((ρ=0·049). Individuals with SARS-CoV-2 positivity at follow-up had longer mean time since diagnosis of HIV infection than those who had negative test results (26·9 years [SD 8·2] vs 16·3 years [9·6]; p=0·023). Clinical, analytical, and radiological presentation of COVID-19 in HIV-infected individuals was similar to that described in the general population. Although the population of infected patients was relatively small, this study represents one of the first to characterize the clinical characteristics of HIV positive patients diagnosed with COVID-19. Overall, no major distinctions in clinical presentation from the general population were identified, and as such no major alterations to approach to treatment were suggested. As factors such as BMI and tenofovir usage had been identified as predictive factors for COVID-19 however, future studies should further investigate any possible interactions between these variables and COVID-19.
1. Patients with haematological malignancies had poorer prognoses than patients with solid tumours, and administration of chemotherapy within 4 weeks of symptom onset was associated with higher case fatality rate.
Evidence Rating: 2 (Good)
Although patients with cancer have been identified as an a vulnerable population during the COVID-19 pandemic, due to illness, immunosuppressive therapy, poor nutrition, and treatment related side effects, the clinical characteristics and prognostic factors of these patients were not well characterized. Researchers attempted to address this knowledge gap in a retrospective multicentre cohort study, analyzing the data of 205 patients with a pathological diagnosis of a malignant tumour and laboratory confirmed SARS-CoV-2. Patients were followed up for a mean duration of 68 days, and by the end of the 78 day study period, all patients had either died or been discharged from the hospital. Severe pneumonia occurred in 52 (25%) patients and the in-hospital case-fatality rate in patients with COVID-19 and cancer was 20%, which was considerably higher than previously reported national fatality rate of 1%. Patients with haematological malignancies had significantly poorer prognoses than did those with solid tumours, with 9 of 22 patients (41%) having passed away versus 31 of 183 (hazard ratio for death 3·28 [95% CI 1·56–6·91]; log rank p=0·0009). Interestingly, analysis had also shown receiving chemotherapy within 4 weeks before symptom onset (odds ratio [OR] 3·51 [95% CI 1·16–10·59]; p=0·026) and male sex (OR 3·86 [95% CI 1·57–9·50]; p=0·0033) as significant risk factors for death during hospital stay. No major distinctions in clinical presentation were noted, with fever being the most common symptom, followed by cough, fatigue, and shortness of breath. Although results were not directly compared to a matched control group, the study makes a considerable effort to characterize COVID-19 in cancer patients and demonstrates a significant case mortality rate in this patient population. Haematological malignancies, male sex, and recent chemotherapy appear to be associated with higher mortality rates, and may be used as tools to help clinicians risk stratify early in the clinical setting.
Image: PD
©2020 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.


![2MM: AI Roundup- AI Cancer Test, Smarter Hospitals, Faster Drug Discovery, and Mental Health Tech [May 2nd, 2025]](https://www.2minutemedicine.com/wp-content/uploads/2025/05/Untitled-design-350x250.png)