2 Minute Medicine Rewind June 15 – June 21, 2015
Ezetimibe Added to Statin Therapy after Acute Coronary Syndromes
HMG-CoA reductase inhibitors (statins) lower LDL cholesterol levels and reduce the risk of cardiovascular events. Ezetimibe is a non-statin lipid lowering medication that reduces the absorption of cholesterol in the intestines and can further decrease LDL cholesterol levels when added in addition to statins. In this double blind, randomized control trial, 18 144 patients in 39 different countries who had been hospitalized in the preceding ten days for an acute coronary syndrome (ACS) and had documented dyslipidemia were randomized to receive either simvastatin 40 mg + ezetimibe 10 mg (n = 9067) or simvastatin 40 mg + placebo (n = 9077). Patients in each group were followed for 6 years with the primary outcome measure being a composite of cardiovascular death, a major coronary event (nonfatal myocardial infarction, unstable angina requiring hospitalization, or coronary revascularization), or nonfatal stroke. The event rates for the primary end point were 32.7% in the simvastatin + ezetimibe group and 34.7% in the simvastatin + placebo group (ARR 2.0 percentage points; HR, 0.936; 95% CI, 0.89 – 0.99; p = 0.016). The risk of myocardial infarction (HR, 0.87; p = 0.002) and ischemic stroke (HR, 0.79; p = 0.008) were significantly lower in the simvastatin + ezetimibe group. The rate of composite end point of death from cardiovascular causes, myocardial infarction, or stroke (HR, 0.90; p – 0.003) was significantly lower in the simvastatin-ezetimibe group, as was the rate of major vascular events (HR, 0.928; p = 0.007). The findings in this study are consistent with previous studies showing that a greater reduction in LDL cholesterol levels results in a significant reduction in cardiovascular events.
Readmission Destination and Risk of Mortality after Major Surgery: An Observational Cohort Study
Hospital readmissions after major surgery are a common occurrence in the USA. Depending on the type of post-operative complication, a patient’s proximity to a particular hospital, and access to healthcare resources, patients may end up being seen and assessed for a post-op complication at a hospital different from the one where their original surgery took place. In this retrospective cohort study, investigators gathered information from 9, 440, 5503 Medicare beneficiaries in the United States who required hospital readmission within 30 days after undergoing one of 12 major operations. Logistic regression models were used to measure associations between readmission destination and risk of 90-day mortality for patients who suffered a post-operative complication and needed hospital readmission. It was found that readmission to the index hospital was more likely if the post-operative complication was of a surgical nature (23%) compared to a non-surgical nature (13%; p < 0.0001). It was also found that readmission to the index hospital was associated with a 26% lower risk of 90-day mortality when compared to readmission to a non-index hospital (OR 0.74, 95% CI 0.66-0.83, p < 0.0001), suggesting improved survival for patients readmitted to hospital after major operations if they return to the hospital where their surgery took place. These findings could have important implications with respect to patient follow up post-operatively and the regional centralization of surgical care.
Vitamin D and Calcium Attenuate Bone Loss With Antiretroviral Therapy Initiation: A Randomized Trial
Antiretroviral therapy (ART) for the management of HIV infection has led to an incredible decrease in the incidence of AIDS-defining conditions and has allowed us to treat HIV as a manageable chronic illness as oppose to a terminal disease. Despite the incredible pharmacological advances, ART continues to have a great deal of side effects, including an up to 6 % loss of bone mineral density (BMD), leading to an increased risk of osteoporosis and fragility fractures in patients taking ART. Given that the lifespan of those with well-managed HIV is now approaching that of seronegative persons, we will likely see an increase in fragility fractures in this population. In this prospective, randomized, double-blind, placebo-controlled study, 165 HIV positive, ART-naive patients were randomly assigned to receive either, 4000 IU of Vitamin D3 + 500 mg of Calcium (n = 79) or placebo (n = 86) with initiation of ART (efavirenz/emtribitabine/tenofovir) to ascertain whether or not the addition of calcium and vitamin D supplementation has an effect on bone health in patients on ART. The primary end point was percentage of change in total hip BMD from baseline at 48 weeks. It was found that the addition of vitamin D3 + calcium with the initiation of ART mitigates BMD loss, with the decline in total hip BMD being smaller in the Vitamin D3 + calcium group (median –1.36%; IQR –3.43% to 0.50%) when compared to the placebo group (median –3.22%; IQR –5.56% to –0.88%) at 48 weeks (p = 0.0004). This study is the first to show that vitamin D3 and calcium supplementation is an effective was of promoting bone health in persons with HIV on ART.
Since its implementation in 2006, Medicare prescription drug insurance benefit (Part D) has allowed for increased access to prescription drugs for millions of older adults and adults with disabilities. Easy access to necessary medications is an important aspect of ensuring the proper management of medical conditions, however more research is needed to ascertain whether or not the implementation of Part D has had any effect on the overall health outcomes of the Medicare population. In this population-level longitudinal time-series analysis, generalized linear models were used to examine changes in self-reported health status, limitations in activities of daily living (ADL’s), emergency department visits, hospital admissions, and mortality in a sample of Medicare beneficiaries from 2000 to 2010 (n = 56, 293). Investigators found no clinically or statistically significant reductions in emergency department visits or hospital admissions, and no significant improvements with respect to overall health status, activities of daily living, or mortality in Medicare Part D recipients, 5 years after its implementation. These findings are inconsistent with previous studies, which were largely based on claims data, and did find improved population health outcomes. The fact that this study used self-reported data may account for some of the differences between the two types of study findings however more research is needed in order to understand these differences.
The legalization of medical marijuana is frequently debated and the relationship between the legalization of medical marijuana as it relates to marijuana use in adolescents is usually at the forefront of this debate. It is often argued that the legalization of marijuana for medical purposes conveys a message of acceptability that may increase its use amongst impressionable populations. In this cross-sectional study, researchers analyzed data from self-administered questionnaires that included questions on marijuana between 1991 and 2014 (n = 1, 098, 270 adolescents) in order to assess marijuana use in the 30 days prior to questionnaire completion (primary outcome). The investigators sought to identify whether or not marijuana use was higher in states that passed medical marijuana laws (up to 2014) and how the passage of medical marijuana laws affected risk of marijuana use in adolescents. It was found that marijuana use was more prevalent in states that passed medical marijuana laws when compared to other states (adjusted prevalence 15.87% vs 13.7%; adjusted OR 1.27, 95% CI 1.07 – 1.51; p = 0.0057). No significant difference was found with respect to risk of marijuana use in states prior to- and post- passage of medical marijuana laws (adjusted prevalence 16.25% vs 15.45%; adjusted OR 0.92, 95% CI 0.82 – 1.04; p = 0.185). The findings in this study are consistent with findings in similar studies, which suggest that the passage of state medical marijuana laws does not increase the use of marijuana amongst adolescents. More research is needed in order to identify factors that may contribute to marijuana use in adolescents.
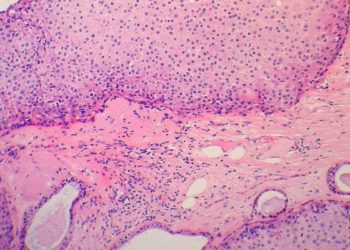
Image: PD
©2015 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.