2 Minute Medicine Rewind June 27, 2016
Statins are recommended in the long-term management of low-density lipoprotein cholesterol (LDL-C) levels in patients with stable ischemic heart disease (IHD). However, clear and consistent LDL-C by clinical practice guidelines have yet to established. In this observational cohort study, 31,619 IHD patients with at least 1 year of adherence to statin therapy were followed up to quantify the relationship between observed LDL-C levels and cardiovascular outcomes. Patients were stratified according to the first observed LDL-C level achieved after 1 year of statin use, where a LDL-C levels <70.0mg/dL, 70.1-100.0mg/dL and 100.1-130.0mg/dL were considered low, moderate and high, respectively. Researchers found that rates of major adverse cardiac events (MACEs) were similar in the low and moderate LDL-C groups, where patients with a low LDL-C did not confer a significant benefit compared to those with a moderate LDL-C (HR 1.02, 95% CI 0.97 to 1.07, p=0.54). Compared to patients with high LDL-C, however, those with moderate LDL-C were significantly less likely to experience a MACE (HR 0.89, 95% CI 0.84 to 0.94, p<0.001). This study therefore shows that patients with LDL-C levels of 70.1-100.0mg/dL using statins are significantly less likely to experience MACEs compared to those with high LDL-C levels. However, these patients do not further lower their risk by lowering their LDL-C levels below 70.0mg/dL.
Patients with breast cancer report high levels of physical and psychological symptoms after treatment. Persistent post-treatment pain is of particular concern, where up to 20% of women experience moderate to severe pain several years after breast cancer surgery. Pain is often neuropathic, but also related to sensory, cognitive and affective factors that influence the patient’s pain experience. Mindfulness based therapy has been shown to reduce anxiety and depression, and improve quality of life in cancer populations. In this randomized controlled trial, 129 patients were randomized to an 8-week mindfulness-based cognitive therapy (MBCT) or waitlist, to assess the effect of MBCT on late post-treatment pain in women treated for primary breast cancer. The short-form McGill Pain Questionnaire 2 (SF-MPQ-2) and Present Pain Intensity (PPI) were used to measure the primary outcome. Researchers found that MBCT participants reported significantly reduced pain intensity (p = 0.026) and neuropathic pain (p = 0.036). However, upon statistically correcting for comparisons of multiple outcomes, only pain intensity remained statistically significant (p = 0.002). This study therefore shows that MBCT may be used in the reduction of pain intensity in breast cancer patients with late post-treatment pain.
Prediction of bladder outcomes after traumatic spinal cord injury: a longitudinal cohort study
The majority of patients with spinal cord injury (SCI) develop neurogenic bladder dysfunction. In addition to the tremendous effects this has on quality of life, patients are also at an increased risk of developing related complications, including recurrent urinary tract infections (UTIs), urethral strictures, calculus disease, hydronephrosis, and ultimately, renal failure. The early prediction of bladder outcomes is essential in counseling patient and planning neurological management. In this longitudinal cohort study, the authors used data on 1250 patients from the European Multicenter Study about Spinal Cord Injury (EMSCI) to derive 2 prediction models for urinary continence and complete bladder emptying 1 year after traumatic spinal cord injury. The models were subsequently validated using an independent cohort of 111 patients with traumatic SCI. Researchers found that the full model for the prediction of urinary continence and complete bladder emptying relied on the patient’s lower extremity motor score (LEMS), light-touch sensation in the S3 dermatome, and Spinal Cord Independence Measure (SCIM) subscale for respiration and sphincter management. The area under the receiver operating curve (aROC) for this full model was 0.936 (95% CI 0.922 to 0.951). The simplified model relied solely on LEMS, resulting in an aROC of 0.912 (95% CI 0.895 to 0.930). External validation of the full and simplified models supported a high predictive power, where the aROCs were 0.965 (95% CI 0.934 to 0.996) and 0.972 (95% CI 0.943 to 0.999), respectively. This study therefore demonstrates that certain variables used in the classification of spinal cord injury and measures of independence can be used in the early prediction urinary continence and complete bladder emptying. This has important implications in counseling patients, setting rehabilitation goals and offering patients tailored interventions.
High rates of perinatal mortality are associated with a lack of quality antenatal, obstetric and early neonatal care. The United Nations has identified key medical interventions or ‘signal functions’ in basic emergency obstetric neonatal care that must be provided by all skilled birth attendants, including neonatal resuscitation. Providing quality care, however, presents as a challenge as most deliveries and emergencies in healthcare facilities take place peripherally, where healthcare workers often lack the training required in the management of complex emergencies. Mobile phone apps have the potential to overcome some of these challenges. In this cluster-randomized controlled trial, 73 healthcare facilities in Ethiopia were randomized to the mobile phone intervention or standard care to determine the effect of a safe delivery app (SDA) on the knowledge and skills of healthcare workers in neonatal resuscitation and perinatal mortality. Researchers found that the intervention was associated with a non-significant reduction in perinatal mortality (OR 0.76, 95% CI 0.32 to 1.81). However, after 6 and 12 months from baseline, healthcare workers’ skill scores did improve, where the mean difference between scores of intervention and control healthcare workers was 6.04 (95% CI 4.26 to 7.82) at 6 months and 8.79 (95% CI 7.14 to 10.45) at 12 months. This corresponded to improvements of 80% and 107% at 6 and 12 months, respectively. Knowledge scores also significantly improved in the intervention group at 6 months (mean difference 1.67, 95% CI 1.02 to 2.32) and 12 months (mean difference 1.54, 95% CI 0.98 to 2.09), corresponding to improvements by 39% and 38%, respectively. This study therefore shows that the SDA is an effective method of improving and sustaining healthcare workers’ knowledge and skills in neonatal resuscitation. This has important implications in the delivery of quality obstetrical care in settings with limited resources and continuing education.
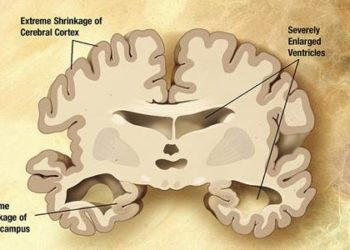
Cerebral Amyloid Angiopathy Is Associated With Executive Dysfunction and Mild Cognitive Impairment
Cerebral amyloid angiopathy can manifest in a number of ways, including cognitive impairment. The frequency, severity and cognitive profile of patients with CAA, however, has not been well-studied with neuropsychological testing. Autopsy-based studies have found associations between CAA and declines in global cognition, perceptual speed, episodic and semantic memory, however CAA in these cases was diagnosed after death. In this prospective cohort study, 34 patients with a CAA-related syndrome underwent neuropsychological assessment and magnetic resonance imaging (MRI) to determine the cognitive profile of patients with CAA. Neuropsychological test results in non-demented CAA patients were compared to participants with dementia caused by Alzheimer’s disease, mild cognitive impairment and ischemic stroke. Researchers found that the mean test scores in CAA participants were significantly lower than normal values for memory (p = 0.02), executive function (p < 0.001) and processing speed (p < 0.001). In addition, 79% of CAA patients had clinical cognitive concerns, meeting the criteria for mild cognitive impairment. Compared to patients with Alzheimer’s dementia, CAA patients performed better on episodic memory, but were similar with respect to executive function and processing speed. This study therefore demonstrates the high prevalence of mild cognitive impairment among patients with CAA, with deficits in memory, executive function and processing speed.
Image: PD
©2016 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.



![Nanoparticle delivery of aurora kinase inhibitor may improve tumor treatment [PreClinical]](https://www.2minutemedicine.com/wp-content/uploads/2016/02/20541_lores-75x75.jpg)

