2 Minute Medicine Rewind March 13, 2023
1. In this randomized target trial, molnupiravir was found to be associated with a reduced risk of hospital admission and death at 30 days in adults with a SARS-CoV-2 infection and at least one risk factor for progression to severe COVID infection.
2. Molnupiravir was found to be associated with a reduced risk of hospital admission and death at 30 days regardless of vaccination status.
Evidence Rating Level: 2 (Good)
Previous evidence regarding the efficacy of molnupiravir in adults with COVID-19 infections has been limited; a previous trial showed that molnupiravir reduced hospital admission or death in unvaccinated adults with COVID-19, but the trial was conducted in the pre-omicron era. A recent trial in vaccinated adults showed that molnupiravir did not reduce the frequency of covid-19 related hospital admissions or death, but the trial excluded people at the highest risk of adverse outcomes. Overall, due to the limited nature of previous evidence, this emulated randomized target trial aimed to estimate whether molnupiravir offers a benefit over no treatment in reducing hospital admission or death at 30 days in adults with SARS-CoV-2 infection in the community during the omicron predominant era who have at least one risk factor for progression to severe COVID-19 infection. This randomized target trial included patients with confirmed SARS-CoV-2 infection between January 5 and September 30 2022 with at least one risk factor for progression to severe COVID-19. Data were collected from the Veterans Affairs healthcare database in the United States. The primary outcome studied was the composite of all-cause hospital admission and death. In total, 85 998 adults were enrolled in this trial; 7 818 (9.1%) patients were eligible for and treated with molnupiravir, and 78 180 (90.9%) patients received no treatment. Molnupiravir treatment was found to be associated with a reduction in hospital admission or death at 30 days (relative risk 0.72; 95% confidence interval 0.64 – 0.79). The rate of hospital admission or death at 30 days was 2.7% (95% CI, 2.5% – 3.0%) for the molnupiravir group and 3.8% (95% CI, 3.7 – 3.9%) for the no-treatment group, with an absolute risk reduction of 1.1% (95% CI, 0.8% – 1.4%). Separate emulated trials suggested that molnupiravir was effective against hospital admission or death at 30 days in unvaccinated adults, adults who had received one or two vaccine doses, and those who had received a booster dose. In addition, molnupiravir was found to be effective regardless of prior SARS-CoV-2 infection. Overall, this emulated randomized target trial found that Molnupiravir is effective in reducing hospital admission or death at 30 days in adults regardless of vaccination status during the omicron-predominant era. A limitation of this study is the population, consisting mostly of white males, which affects the generalizability of the data. This randomized study is an important addition to a growing body of evidence surrounding anti-viral medications and focuses on an omicron-predominant era, which would be more representative of the current subvariants of COVID-19.
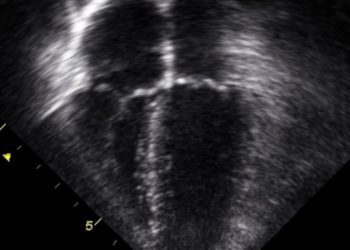
Evaluation of Pulmonary Fibrosis Outcomes by Race and Ethnicity in US Adults
1. In this retrospective cohort study, Black patients with pulmonary fibrosis (PF) were found to have a younger age of diagnosis, first hospitalization, lung transplant, and death when compared with Hispanic and White patients.
2. Black patients were found to have a lower crude mortality rate ratio when compared to White and Hispanic patients.
Evidence Rating Level: 2 (Good)
Recently, death rates from chronic respiratory diseases have recently increased, largely driven by the rising burden of interstitial lung diseases (ILD). Pulmonary fibrosis (PF), a form of ILD, accounts for the highest increase in mortality rates. Racial and ethnic minority populations face the greatest risk of morbidity and mortality from health disparities; Black patients have high rates of respiratory impairment and may have differential survival in ILD when compared to White individuals. This study sought to evaluate the age of PF-related outcomes and the survival patterns among White, Black, and Hispanic participants with PF. This cohort study was conducted using the Pulmonary Fibrosis Foundation (PFF) patient registry as the primary cohort, containing data on more than 2000 patients across the United States. Outcomes included clinically relevant milestones of ILD, including diagnosis, hospitalizations, lung transplant, and all-cause mortality. In total, 5275 patients with a diagnosis of PF were included from January 2003 to April 2001. There were 488 (10.2%) Black patients, 318 (6.7%) Hispanic patients, and 3985 (83.2%) White patients. At study enrollment, Black patients with PF were least likely to be male and had the highest body mass index, while Hispanic and White patients were predominantly male. With respect to outcomes, Black patients had a lower crude mortality rate ratio when compared to White patients (P<.001), while Hispanic patients had a similar mortality rate ratio to White patients. Mean hospitalization events per person were highest among Black patients when compared with Hispanic and White patients (P<.001). Black patients generally had the youngest mean age at first hospitalization, lung transplant, and death with PF when compared to Hispanic and White patients (P<.001). Overall, this study demonstrated racial and ethnic disparities in PF outcomes; notably, Black patients with PF were diagnosed and hospitalized, underwent lung transplants, and died at a younger age than White and Hispanic patients. Mortality rates appeared to be lower in Black individuals than Hispanic and White individuals. A major limitation of this study is that differences in ILD subgroups (i.e., connective tissue-related versus idiopathic) may influence the prevalence of hospitalizations and lung transplants. Further research is required to identify and mitigate underlying responsible factors for this racial and ethnic disparity.
1. In this phase II randomized clinical trial, treatment of patients with locally advanced esophageal squamous cell carcinoma (ESCC) with socazolimab prior to minimally invasive esophagectomy achieved lower major pathological response (MPR) rates than treatment with placebo, though this difference did not reach statistical significance.
2. The proportion of primary tumours at the ypT0 stage in the socazolimab and cisplatin group was significantly higher than in the placebo and cisplatin group.
Evidence Rating Level: 1 (Excellent)
The prognosis for esophageal cancer is poor, with a 5-year survival rate currently less than 20%. Surgery-based combination therapy is the primary treatment for non-metastatic esophageal squamous cell carcinoma (ESCC), and neoadjuvant concurrent chemotherapy is an essential part of preoperative treatment that can improve resection and survival rates. Programmed cell death ligand 1 (PD-L1) inhibitors are a relatively overlooked checkpoint inhibitor for ESCC; emerging evidence has shown promising results of socazolimab, a novel humanized IgG1 monoclonal antibody against PD-L1, in patients with small-cell lung cancer and cervical cancer. Thus, this multicenter, randomized, double-blind phase II study was designed to assess the feasibility, safety, and efficacy of neoadjuvant socazolimab and chemotherapy followed by minimally invasive esophagectomy in patients with resectable locally advanced ESCC. This study was conducted at six hospitals in China, and patients that were recruited In phase II were randomly divided in a 1:1 ratio between the experimental (socazolimab + nab-paclitaxel + cisplatin (TP)) and control (placebo + TP). All patients underwent video-assisted thoracoscopic esophagectomy between 4 and 6 weeks after neoadjuvant treatment. The main endpoint was the major pathological response (MPR) rate. Overall, 64 patients were recruited in phase II and were equally divided into the two arms, with no significant clinical characteristics found between the two groups. Of patients who underwent surgery, 29 (100.0%) in the Socazolimab + TP group and (96.6%) in the Placebo + TP group reached R0. Furthermore, with respect to the primary endpoint, 20 (69.0%) patients in the Socazolimab + TP group and 18 (62.1%) patients in the Placebo + TP group reached MPR (P=.581). Notably, the proportion of primary tumours at the ypT0 stage in the Socazolimab + TP group was considerably higher than in the Placebo + TP group (37.9% vs. 3.5%; P=.001). Overall, in this randomized controlled trial, treatment with socazolimab, nab-paclitaxel, and cisplatin demonstrated a better antitumour effect than the placebo with cisplatin, though this difference was not statistically significant. However, the proportion of patients achieving complete regression of the primary tumour was significantly higher in the socazolimab and cisplatin group versus the placebo and cisplatin group, indicating the PD-L1 inhibitor approach enhanced regression of the primary tumour. A major limitation of this study is the short follow-up time, as we are not yet able to appreciate any differences between median survival between the two groups. This study is an important addition to the growing body of evidence surrounding PD-L1 inhibitors and their use in ESCC.
1. In this prospective cohort study, age was found to be the most prominent risk factor for the development of atrial fibrillation (AF) in adults between 40 to 69 years old in the United Kingdom.
2. Both risk factor burden and genetic predisposition were found to play a pivotal role in the risk of developing AF, especially among male participants and those of a younger age.
Evidence Rating Level: 2 (Good)
Atrial fibrillation (AF) is one of the most common cardiac arrhythmias, posing a significant worldwide health and economic burden. Current risk prediction tools may not be up to date with current rates and risk factors for AF. The estimate of the 10-year risk of AF should integrate modifiable risk factors as well as genetic predisposition; this study aims to estimate the 10-year risk of AF in various subgroups with different genetic and clinical factors and to evaluate the combined effects and potential interactions of risk factors and genetic predisposition on the incidence of AF. Participants aged 40 – 69 years old enrolled from 2006 to 2010 in the UK Biobank were included in the analysis. They were divided into three categories: index ages 45, 55, and 65 years according to the ages at assessment. Participants free of AF were followed up from the late dates of their index age until the first AF occurrence, death, loss to follow-up, end of ten-year follow-up, or March 31, 2021. The primary outcome studied was the incidence of AF, including both atrial fibrillation and flutter. In total, 348904 participants were included in the statistical analysis, defined by index ages of 45 (n = 84,206), 55 (n = 117,520), and 65 (n = 147,178) years. The overall 10-year risks of AF were 0.67% (95% CI, 0.61% – 0.73%) for index age 45 years, 2.05% (95% CI, 1.96 – 2.13%) for index age 55 years, and 6.34% (95% CI, 6.21% – 6.46%) for index age 65 years. History of myocardial infarction or heart failure had the strongest association with a 10-year risk of AF at each index age, followed by diabetes mellitus and alcohol consumption. Generally, participants with a higher risk factor burden or higher polygenic risk score (based on their genetic predisposition to AF) had a higher risk of developing AF. Overall, this large prospective study identified the overall 10-year risks of AF in the study population, as well as the variation depending on risk factor burden and genetic predisposition. The 10-year risk was highest in men with high PRS and elevated risk factor burden at each index age. There are three clinical implications; first: risk factor burden and genetic predisposition are pivotal in the risk of AF; second: age was the most prominent risk factor for AF; and third: at younger ages, earlier onset of AF may result from interactions of elevated risk burdens and PRS. A major limitation of this study was that not all potential risk factors for AF were included in this study, and an under-measured risk factor burden may potentially affect the results. However, this large prospective study is an important step to better characterize the risk of developing AF, including genetic factors, especially with current AF incidence rates.
Comparison of Symptoms Associated With SARS-CoV-2 Variants Among Children in Canada
1. In children presenting to the emergency department (ED) with a COVID-19 infection, children with the Omicron variant were more likely to present with fever, lower respiratory symptoms, and systemic manifestations than children with earlier variants.
Evidence Rating Level: 2 (Good)
During the COVID-19 pandemic, the emergence of variants of concern (VoC) with varying transmissibility patterns and symptoms have influenced the course of the pandemic. The most recent VoC, Omicron, has a propensity to infect the upper airways, with differing symptoms and a lower mortality compared to the delta variant. However, there have been no reports of symptom prevalence and disease severity of the latest VoC, and this study aimed to quantify and compare symptoms, emergency department chest radiography, treatment, and disposition across dominant SARS-CoV-2 variants. This prospective observational cohort study recruited children tested for acute SARS-CoV-2 infection who presented for care at a Canadian urban pediatric emergency department between August 2020 and February 2022. The primary outcome studied was the presence and number of presenting symptoms from illness onset until study enrollment. Overall, 1440 participants had positive test results for SARS-CoV-2 infection. Testing for VoC was performed on 388 participants (26.9%), which identified 158 (40.7%) Alpha, 177 (45.6%) Delta, and 46 (11.9%) Omicron variants. Among the participants, fever, cough, and rhinorrhea were the most common individual symptoms. Patients with Alpha variant infection were least likely to be drowsy, and have conjunctivitis, oral changes, rhinorrhea, and sore throat. Patients with Delta variant infection most often had conjunctivitis, cough, and upper respiratory tract infections. Patients with Omicron variant infection most often experienced drowsiness, fever, and shortness of breath. In total, patients with the Alpha variant had the fewest total number of symptoms. Further analysis found that the Omicron and Delta infections were often associated with fever and cough. In addition, notably, the Delta infection was associated with the reporting of upper respiratory tract symptoms, while the Omicron infection was associated with lower respiratory tract symptoms. Overall, among children positive for SARS-CoV-2 who presented for care in pediatric emergency departments across Canada, symptom profiles differed based on etiologic variants. Children with Omicron infection were more likely to present with fever, lower respiratory tract symptoms, and systemic manifestations when compared to earlier variants. A major limitation of this study is the selection bias, as children with symptoms associated with COVID-19 infection were more likely to be tested. The findings of this study are important to characterize the symptoms of the current predominant strain to guide management in children presenting to the emergency department with suspected COVID-19 infection.
Image: PD
©2023 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.