2 Minute Medicine Rewind March 25, 2024
1. This case-control study found that in patients with atrial fibrillation concomitant Serotonin Reuptake Inhibitor (SSRI) and Oral Anticoagulants (OAC) was associated with an increased risk of major bleeding compared with OAC use alone.
2. This increased risk was highest in the first 30 days of continuous, concomitant use.
Evidence Rating Level: 2 (Good)
Antidepressants, especially SSRIs, are widely prescribed, raising concerns about their interaction with OACs and the risk of major bleeding. Utilizing the UK Clinical Practice Research Datalink, this case-control study investigated whether concomitant SSRIs and OACs use was associated with the risk of major bleeding compared with OAC use alone among patients with AF. 331 305 patients with an incident diagnosis of AF between January, 1998, and March, 2021 and a prescription for an OAC (apixaban, dabigatran, edoxaban, rivaroxaban, or warfarin) after AF diagnosis were identified. 42 190 patients (mean [SD] age, 74.2 [9.3] years; 59.8% men) were identified as cases—patients with a first recorded diagnosis of major bleeding during follow-up—and were matched to 1 156 641 controls (mean [SD] age, 74.2 [9.3] years; 59.8% men). Concomitant SSRIs and OACs use was associated with a 33% higher risk of major bleeding compared to OAC use alone (IRR: 1.33; 95% CI: 1.24-1.42). The risk peaked within the initial 30 days of continuous use (IRR: 1.74; 95% CI: 1.37-2.22) and declined afterward. Age, sex, history of major bleeding, chronic kidney disease, and SSRI potency did not alter the risk. Moreover, the risk remained elevated for concomitant SSRIs with both DOACs (IRR: 1.25; 95% CI: 1.12-1.40) and VKAs (IRR: 1.36; 95% CI: 1.25-1.47) compared to DOACs and VKAs alone, respectively. Overall, these findings suggest that concomitant SSRI and OAC use was associated with an increased risk of major bleeding compared with OAC use alone, underscoring the need for close monitoring, especially during initial SSRI-OAC use, to mitigate bleeding risks.
1. This retrospective cohort study found that immediate weight-bearing following clavicle fracture fixation in patients with concurrent lower extremity trauma does not impact rates of hardware failure (HWF) or fracture union, compared with non-weight bearing (NWB) patients with isolated clavicular fractures.
Evidence Rating Level: 2 (Good)
Clavicle fractures are increasingly treated with open reduction internal fixation (ORIF). Postoperative care often involves 6 weeks of NWB, but in polytrauma cases with lower extremity injuries, NWB is challenging. This study compared immediate weight-bearing post-ORIF with standard NWB protocol to assess the impact on complications. 39 polytrauma patients, with concurrent lower extremity fractures, who used a walker or crutches for weight-bearing post-ORIF of their clavicle, were age (44±17 years) and sex (72% men) matched with a control group of 39 patients who followed a progressive rehabilitation protocol that restricted full weight-bearing until 6 weeks after their isolated clavicular fracture ORIF. There were no significant differences in plate number, type, fixation cortices, or screw count between groups (P > 0.05). However, there were notable variations in plate positioning and fixation type (P < 0.05), with the weight-bearing as tolerated (WBAT) group exhibiting higher proportions of isolated anterior plating and 90-90 fixation, while the NWB group more frequently received isolated superior plating. Additionally, there were differences in overall construct types (P = 0.03), with the WBAT group having more compression plating and the NWB group more commonly treated with lag screws with neutralization plates and bridge plating. There was no difference in overall HWF (WBAT group: 1 patient vs. NWB group: 2 patients; P = 0.49) with both groups having one patient (2.5%) necessitating surgical intervention due to acute hardware failure (P = 1.0). Final union rates showed no significant difference between cohorts (P = 1.0). Overall, this study found that WBAT after clavicle ORIF in patients with concomitant lower extremity trauma does not increase HWF or impact fracture union. However, these results should be considered in the context of between-group variations in plate positioning, fixation type, and construct type, which may represent a potential treatment bias, as surgeons might have opted for stronger constructs for polytrauma patients in anticipation of weight-bearing through their fixation.
1. This retrospective cohort study found that in one surgeon’s practice, administration of vancomycin/tobramycin local antibiotic powder (LAP) after open treatment of fractures resulted in an 8.3% reduction in deep surgical site infections (SSIs) compared with no LAP procedures.
Evidence Rating Level: 2 (Good)
Conflicting data exist regarding LAP effectiveness in reducing SSIs in orthopedic surgery. While the VANCO trial showed no significant reduction in deep SSIs with vancomycin LAP, post hoc analysis suggested a decrease in gram-positive infections offset by gram-negative ones. To address this, the senior author began routinely using vancomycin and tobramycin LAP in high infection risk cases, but by 2020, found no difference in SSI rates (13% vs. 10%; P = 0.4), prompting LAP cessation. This study aimed to assess SSI rates post-LAP cessation and compare LAP and non-LAP groups using propensity-matching to control for selection bias. Vancomycin and tobramycin LAP was applied in 36.7% (n = 114) of procedures before stopping its use, after which 342 procedures were performed without LAP. Prematch analysis of procedures demonstrated that the LAP use was associated with higher BMI (MD 1.2, 95% CI, 0.09–2.4; P = 0.03), external fixation (PD 8.5%, 95% CI, 1.6%–16.2%; P = 0.005), longer operative times (MD 56.0 minutes, 95% CI, 39.0–74.0; P < 0.0001), and greater estimated blood loss (MD 70.0, 95% CI, 50.0–100.0; P < 0.0001), compared with procedures that did not receive LAP. After 1:1 propensity matching to control for the above differences there were no observed differences in patient, injury, or operative characteristics between groups. Following matching, LAP procedures showed no difference in superficial SSIs and were less likely to have deep SSIs (PD −8.3%, 95% CI: −16.2% to −0.2%; P = 0.04). Overall, these findings suggest that vancomycin and tobramycin LAP reduced deep SSI rates after open fracture treatment, supporting LAP use in high-infection
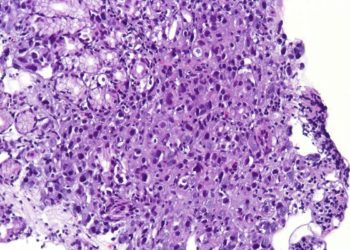
Contemporary national outcomes of hyperbaric oxygen therapy in necrotizing soft tissue infections
1. This retrospective cohort study found that the addition of hyperbaric oxygen therapy (HBOT) to surgery in patients with necrotizing soft tissue infections (NSTIs) reduced mortality, amputation and non-home discharges.
2. These effects were accompanied by longer hospital stays and higher costs.
3. In a subgroup analysis of patients with sepsis, the effects of decreased mortality, amputation, and non-home discharges persisted with no impact on length of stay and costs compared with the non-HBOT group.
Evidence Rating Level: 2 (Good)
NSTIs are life-threatening, managed with early diagnosis, surgery, and antibiotics. The use of additional HBOT remains controversial. A previous analysis of 45,913 patients in the National Inpatient Sample (NIS) from 1988 to 2009 showed a statistically significant reduction in mortality albeit with higher hospitalization costs and longer length of stay This retrospective cohort study aimed to investigate HBOT’s ongoing role in NSTI patients and whether HBOT would still demonstrate beneficial results using data from the latest 2012-2020 update to the NIS. Among 60,481 patients admitted with a diagnosis of NSTI who underwent surgery, 600 (<1%) received HBOT. After adjusting for baseline differences between groups, HBOT was associated with reduced mortality (AOR 0.22, 95% CI 0.09–0.53, P<0.001) and amputation risk (AOR 0.73, 95% CI 0.55–0.96, P = 0.03), with longer hospital stays by 1.6 days (95%CI 0.4–2.7 days) and increased costs by $7,800 (95%CI $2,200-$13,300). HBOT was also correlated with lower odds of non-home discharge, particularly a lower risk of discharge to short-term care facilities (AOR 0.47, 95% CI 0.6–0.95, P = 0.008). In a subgroup analysis including only sepsis patients, the HBOT association with reduced mortality (AOR 0.16, 95% CI 0.06–0.46), reduced amputation risk (AOR 0.42, 95% CI 0.28–0.62), and fewer non-home discharges (AOR 0.73, 95%CI 0.56–0.95) persisted, while length of stay and cost differences between groups were not significantly different. Overall, this study found that HBOT post-surgery decreases mortality, amputation rates, and non-home discharges, with a tradeoff of increase to costs and length of stay. These findings support the use of HBOT in patients with NSTIs, particularly in those with sepsis wherein HBOT did not increase length of stay or hospital costs.
1. This prospective cohort study found that confirmed or suspected SARS-CoV-2 infection was associated with decreased rates of clinical pregnancy in those undergoing in vitro fertilization (IVF), intracytoplasmic sperm injection (ICSI), or frozen-thawed embryo transfer (FET).
Evidence Rating Level:1 (Excellent)
Some research suggests SARS-CoV-2 infection has potential influences on embryo development during controlled ovarian stimulation and increased risks during pregnancy. However, the impact of SARS-CoV-2 infection shortly after embryo transfer in IVF, ICSI or FET is unexplored. This prospective cohort study aims to investigate its effect on the clinical pregnancy rate in women receiving assisted reproductive technology (ART). 1330 patients undergoing embryo transfer in IVF/ICSI/FET were analyzed. Patients were divided into three groups: the diagnosed group, with 51.6% (n = 687) testing positive for SARS-CoV-2 RNA or antigen; the suspected infection group, comprising 16.4% (n = 219) displaying symptoms but unable to get tested; and the uninfected group, consisting of 32% (n = 424) patients with negative test results and no symptoms. Clinical pregnancy rates were 68%, 63%, and 51% in the SARS-CoV-2 diagnosed, suspected infection, and uninfected groups, respectively (P < 0.001). Ongoing pregnancy rates were 58%, 53%, and 45% in the same respective groups (P < 0.001). No significant differences were found in biochemical pregnancy rate, early miscarriage rate, or ectopic pregnancy rate. Logistic regression analysis demonstrated that vaccination (OR 1.513, 95% CI 1.134–2.019, P = 0.005), especially with three doses (OR 1.804, 95% CI 1.332–2.444, P < 0.001) increased the clinical pregnancy rate. Suspected infection status (odds ratio [OR] 0.618, 95% CI 0.444–0.862, P = 0.005), SARS-CoV-2 symptoms with the occurrence of fever and dizziness/headache (OR 0.715, 95% CI 0.526–0.972, P = 0.032) and short interval (≤ 22 days) between embryo transfer and SarS-CoV-2 infection (OR 3.76, 95% CI 1.92–8.24, P < 0.001) decreased the clinical pregnancy rate. Overall, these findings suggest symptomatic SARS-CoV-2 infection shortly after embryo transfer is not conducive to clinical pregnancy.
Image: PD
©2024 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.