2 Minute Medicine Rewind May 12 – May 19, 2014
Image: PD
In this section, we highlight the key high-impact studies, updates, and analyses published in medicine during the past week.
Pharmacotherapy for Adults With Alcohol Use Disorders in Outpatient Settings
Despite continued high rates of morbidity and early mortality caused by alcohol use disorders (AUDs), less than 10% of patients with AUDs receive medications to assist in reducing alcohol consumption. This can partly be attributed to the fact that the benefits and harms of medications for the treatment of adults with AUDs have never officially been studied and compared.In this meta-analysis, 122 RCTs and 1 cohort study (22,803 patients in total) were reviewed and the numbers needed to treat for benefit (NNTs) or harm (NNHs) were calculated. The review found no statistically significant difference between acamprosate and naltrexone for return to any drinking (RD, 0.02; 95% CI, −0.03 to 0.08) or heavy drinking (RD, 0.01; 95% CI, −0.05 to 0.06). Nalmefene and topiramate, both medications used off-label, were shown to have a moderate association with improvement of consumption outcomes: Nalmefene (heavy drinking days per month: weighted mean difference [WMD], −2.0; 95% CI, −3.0 to −1.0; drinks per drinking day: WMD, −1.02; 95% CI, −1.77 to −0.28) and topiramate (% heavy drinking days: WMD, −9.0%; 95% CI, −15.3% to −2.7%; drinks per drinking day: WMD, −1.0; 95% CI, −1.6 to −0.48). Given both acamprosate and naltrexone were found to equally decrease alcohol consumption, the decision of which medication to used should be based on potential adverse events and availability of treatments.
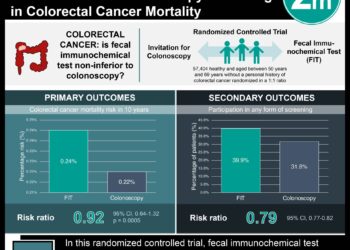
Effect of PET Before Liver Resection on Surgical Management for Colorectal Adenocarcinoma Metastases
Half of patients with colon cancer eventually develop liver metastases and become candidates to undergo hepatic resection with curative intent. However, if unidentified occult metastases are present at the time of surgery, the resection becomes noncurative. Currently, the standard pre-operative workup includes a chest, abdomen, and pelvis CT and a colonoscopy. A pre-operative PET-CT tumors could detect occult metastases given that tumors preferentially take up 18F-fluorodeoxyglucose. In this randomized clinical trial, 404 patients with colorectal cancer and resectable metastases based on CT scans of the chest, abdomen, and pelvis were randomized to PET-CT or control. While 8% of patients in the PET-CT group had a change in surgical management (95% CI, 5.0%-11.9%) based on the findings of the scan, there was no significant difference in the rate of liver resections in both groups (91% vs. 92% in the PET-CT vs. control groups, respectively). In addition, there was no survival change between the 2 groups (hazard ratio, 0.86 [95% CI, 0.60-1.21]; P = .38). Given that a pre-operative PET-CT did not change clinical management or survival in patients with potentially resectable hepatic metastases of colorectal adenocarcinoma, its use it not currently warranted.
Randomized Trial of Posaconazole and Benznidazole for Chronic Chagas’ Disease
While cure rate for acute Chagas disease range between 65 to 80%, that of chronic Chagas disease are as low as 15%. Finding a new treatment for this long neglected disease is overdue. Inhibitors of ergosterol synthesis, such as posaconazole, currently approved for the treatment of invasive fungal infections, are promising given their antiprotozoal activity. In this randomized clinical trial, 78 patients chronic Trypanosomacruzi infection were randomly assigned to receive a high dose of posaconazole (400 mg BID), a low dose of posaconazole (100 mg BID), or benznidazole (150 mg BID), the current standard of care. All but 2 patients tested negative for T. cruzi DNA on rt-PCR assay during the treatment period. Ten months after the end of treatment, per the intention-to-treat analysis, 92%, 81% and 38% of patients treated with low-dose posaconazole, high-dose posaconazole and benznidazole , respectively, tested positive for T. cruzi DNA on rt-PCR assay (P<0.01 for the comparison of the benznidazole group with either posaconazole group). Given the significantly higher rate of treatment failure in the posaconazole groups, benznidazole should continue as the current standard of care.
A Form of the Metabolic Syndrome Associated with Mutations in DYRK1B
Although researchers have successfully identified causative mutations for individual cardiovascular risk factors, the underlying genetic factors that unify their association in the metabolic syndrome remain unknown. In this study, DNA samples from 21 living family members from the three study families with coinheritance of early-onset coronary artery disease, central obesity, hypertension, and diabetes were sequenced and analyzed. A substitution from cysteine for arginine in the DYRK1B gene was found in all family members affected by the clinical syndrome and was absent in unaffected family members and unrelated controls. This finding can be supported by the facts that the protein encoded by DYRK1B inhibits the SHH (sonic hedgehog) and Wnt signaling pathways and consequently enhances adipogenesis, and that DYRK1B promotes the expression of the key gluconeogenic enzyme glucose-6-phosphatase. The newly discovered mutation shows gain-of-function activity. This study has therefore demonstrated a role for DYRK1B in adipogenesis and glucose homeostasis, with a mutation ultimately leading to an increased risk for metabolic syndrome.
Despite receiving high-intensity statin therapy, many patients are unable to achieve the recommended LDL-C goals; in this situation, a nonstatin therapy is recommended for additional LDL-C lowering. Evolocumab is a human monoclonal antibody against PCSK9 that reduces circulating LDL-C levels by preventing the degradation of LDL-C receptors when bound to PCSK9. Given Evolucumab showed LDL-C lowering in phase 2 trials, a phase 3 trial was in order. In this randomized controlled trial, 2067 patients were randomized to a daily, moderate-intensity (atorvastatin [10 mg], simvastatin [40 mg], or rosuvastatin [5 mg]) or high-intensity (atorvastatin [80 mg], rosuvastatin [40 mg]) statin. Four weeks later, patients were then randomized to evolocumab (every 2 weeks or monthly), placebo or ezetimibe in addition to the statin therapies.For both the moderate- and high-intensity statin-treated groups, monthly evolocumab reduced LDL-C levels by 63% to 75% 10-12 weeks after starting treatment. Similar statistics were found in the group receiving evolocumab every other week [reduction of 66% to 75% ]. Adverse events, including back pain, arthralgia, headache, muscle spasms, and pain in extremity, were reported in 36%, 40%, and 39% of evolocumab-, ezetimibe-, and placebo-treated patients, respectively. This study therefore demonstrates the additional LDL-lowering effects of evolocumabin patients already on statin therapy.
©2012-2014 2minutemedicine.com. All rights reserved. No works may be reproduced without written consent from 2minutemedicine.com. Disclaimer: We present factual information directly from peer reviewed medical journals. No post should be construed as medical advice and is not intended as such by the authors or by 2minutemedicine.com. PLEASE SEE A HEALTHCARE PROVIDER IN YOUR AREA IF YOU SEEK MEDICAL ADVICE OF ANY SORT.