2 Minute Medicine Rewind May 2, 2022
1. 3.3% of breast papillomas (BP) without atypia initially managed with radiologic follow-up were upgraded to high-risk or malignancy lesions after subsequent surgical resection.
2. 14.8% of BP without atypia managed with surgical excision were upgraded to high-risk, but not malignancy lesions, on surgical pathology.
3. Factors associated with higher likelihood of upgraded lesions were age ≥60 years and family history of breast cancer.
Evidence Rating Level: 2 (Good)
For breast papillomas (BP) without atypia diagnosed on core needle biopsy, there is uncertainty regarding whether ultrasound imaging is sufficient for follow-up, or if surgical excision is optimal. The argument for excision originates from some studies reporting rates of 50% being upgraded to high-risk lesions, and 0-33% being upgraded to malignancy. However, the 2018 American Breast Surgeons Guidelines recommend imaging follow-up, with a patient-specific risk assessment to decide on whether to perform excision. Therefore, this single-centre retrospective study aimed to identify outcomes of patients who underwent imaging follow-up versus those who underwent surgical excision upfront, and to identify factors associated with with upgraded lesions. The study population consisted of 121 patients with 139 cases of BP from 2011 to 2021, with 81% of cases undergoing imaging follow-up and 19% upfront surgery. Protocols required imaging to be done every 6 months for up to 1 year, and every year for 2 more years. The study found that in the upfront surgery group, 4 patients (14.8%) had lesions upgraded to high-risk lesions from surgical pathology results, with none upgraded to malignancy. 2 of these upgraded patients presented with imaging findings, and 1 presented with nipple discharge, with the remaining patient having unknown presentation. For those in the imaging group, 9 patients (7.4%) had subsequent resection, with 4 patients (3.3%) having lesions upgraded. Of these 4 patients, 2 were upgraded to high-risk lesions, and 2 were to malignancies. As well, 2 presented with new nipple discharge, 1 had discharge and a suspicious intra-mammary lymph node, and 1 had increased size on imaging. Furthermore, associated with upgrade included age ≥60 years (75.0% vs 25.0%, p = 0.049) and family history of breast cancer (87.5% vs 48.1%, p = 0.048). Overall, this study demonstrated that although upgrade to high-risk or malignancy lesions can occur for BP without atypia, this was not common for patients undergoing imaging follow-up (3.3% in this study), and both imaging and clinical presentation changes could identify cases with possibility of upgrade. The study authors recommend radiologic follow-up except for patients with age ≥60 years or family history.
1. For the same NT-proBNP concentration, black men have a 6.7-fold higher absolute predicted risk of incident HF or death in midlife and a 2.7-fold higher risk in late life, compared to white women, even after adjusting for physiologic and social determinants of cardiovascular health.
Evidence Rating Level: 2 (Good)
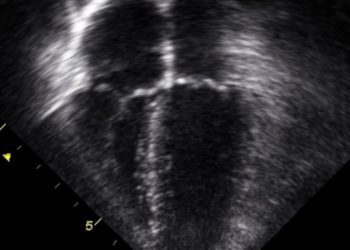
N-terminal pro-B-type natriuretic peptide (NT-proBNP) is a biomarker used for diagnosis, prognosis, and prediction of risk for developing heart failure (HF). Currently, NT-proBNP values are interpreted independent of sex and race. However, circulating NT-proBNP levels have been found to vary by sex and race, with female sex being associated with 165% higher circulating levels than male sex, and Black individuals being associated with 30-40% lower levels than White individuals. It is also unclear whether these differences are due to physiologic determinants, such as cardiac structure and function, kidney function, and body composition. Therefore, this prospective study investigated whether interpreting NT-proBNP values in the context of sex and race would better predict absolute risk of HF, in midlife and late life. The study cohort was taken from the ongoing Atherosclerosis Risk in the Communities (ARIC) study. The participants included were either Black or White, and did not have HF in midlife (visit 2 of the ARIC study, between 1990 and 1992) or in late life (visit 5, between 2011 and 2013). There were 12750 participants at visit 2 (mean [SD] age of 57.3 [5.7], 45% male, 25% Black) and 5191 participants at visit 5. (mean [SD] age of 76.0 [5.2], 41% male, 20% Black). The primary outcome was incident HF, defined as the first hospitalization of HF or death from HF, in the five years of follow-up after each visit. The results showed that in midlife, black men had significantly lower NT-proBNP concentrations compared to white men, black women, and white women (p < 0.001 for all). In late life, black men and black women did not have significantly different NT-proBNP level (p = 0.01), but black men were significantly lower than white men and white women (p < 0.001 for both). Differences in both midlife and late life were significant after adjusting for physiologic determinants, as well as social determinants (such as education and income). Based on guideline NT-proBNP thresholds, there was a difference of 6.7-fold (95% CI 4.6-9.9) in predicted rate of incident HF or death in midlife, and a difference of 2.7-fold (95 CI 1.7-4.1), with black men having the highest and white women the lowest risk. Overall, this study showed that NT-proBNP concentrations interpreted independent of sex and race is associated with differences in risk prediction, with black men having the highest risk and white women the lowest risk, for the same NT-proBNP level.
1. Preterm neonates placed on noninvasive high-frequency oscillatory ventilation (NHFOV) post-extubation were found to have the lowest duration on invasive mechanical ventilation (IMV), compared to nasal continuous positive airway pressure (NCPAP) and nasal intermittent positive pressure ventilation (NIPPV).
2. NCPAP was associated with higher rates of reintubation and fewer ventilator-free days.
Evidence Rating Level: 1 (Excellent)
Invasive mechanical ventilation (IMV) is often required for neonates born preterm, but it is associated with bronchopulmonay dysplasia (BPD), neurologic impairment, and rehospitalization. Therefore, various noninvasive ventilation modalities are used to minimize the duration spent on IMV. The current standard is to use nasal continuous positive airway pressure (NCPAP), but many neonates do not respond and require reintubation. Other modalities include nasal intermittent positive pressure ventilation (NIPPV), which decreases the requirement for IMV compared to NCPAP, and noninvasive high-frequency oscillatory ventilation (NHFOV), which is unconventional but increasing in popularity. This randomized controlled trial conducted at 69 NICUs in China compared the duration spent on IMV after extubation, among neonates using NCPAP, NIPPV, and NHFOV, as well as the need for reintubation and the number of ventilator-free days. In total, 1493 neonates were randomized, with a mean (SD) gestational age of 29.4 (1.8) weeks. The results showed that IMV was longer in the NIPPV (mean difference 1.2, 95% CI 0.01-2.3 days, p = 0.04) and NCPAP (mean difference 1.5 days, 95% CI 0.3-2.7 days, p = 0.01) groups, compared to the NHFOV group, with no significant difference between NIPPV and NCPAP. As well, there were higher rates of reintubation in the NCPAP group compared to NHFOV (risk difference 12.5%, 95% CI 7.5-17.4%, p < 0.001) and compared to NIPPV (risk difference 8.1%, 95% CI 2.9-13.3%, p = 0.003), with no significant difference between NIPPV and NHFOV. Finally, there were significantly fewer ventilator-free days in the NCPAP group than the NIPPV group (median [IQR] difference of -3 [-6 to -1] days, p = 0.01). Overall, this study demonstrated that NHFOV is associated with the least duration on IMV, and NCPAP is associated with higher rates of reintubation and fewer ventilator-free days.
1. Favourable lifestyle factors such as no or moderate alcohol consumption, no smoking, regular physical activity, and healthy diet, attenuated the risk of developing gout in patients with low, middle, and high genetic risk.
Evidence Rating Level: 3 (Average)
Gout is an inflammatory arthritic condition characterized by monosodium urate crystals depositing in joints, due to high levels of uric acid. Studies have shown that genetic factors influence the risk of developing gout, with 30% heritability and over 20 genetic loci being identified. As well, lifestyle factors influence this risk too, such as alcohol, diet, smoking, and exercise. Therefore, this current cohort study investigated whether positive lifestyle factors can dampen the effect of genetic factors on risk of developing gout. The cohort was taken from the UK Biobank, and the 416,481 included participants did not have prevalent gout at baseline, and were of white British ancestry (as other demographics did not have genetic information available). Lifestyle information was collected from patient questionnaires, and patients were categorized into three groups depending on their number of aforementioned healthy lifestyle factors: Unfavourable (0-1), intermediate (2), and favourable (3-4). Additionally, a polygenic risk score was calculated, for which participants were divided into low risk (lowest tertile), middle risk (tertile 2), and high risk (highest tertile) genetic categories. The study found that each of the lifestyle factors was associated with a diminished risk of developing gout: No or moderate alcohol consumption was associated with a lower risk by 33% (hazards ratio 0.67, 95 %CI 0.63-0.70) lower risk, not smoking by 11% (HR 0.89, 95% CI 0.84-0.93), regular physical activity by 10% (HR 0.90, 95% CI 0.86-0.95), and healthy diet by 10% (HR 0.90, 95% CI 0.85-0.94). Furthermore, favourable lifestyle (compared to unfavourable) was associated with reduced risk among individuals with a low genetic risk (HR 0.64, 95% CI 0.56-0.73), middle genetic risk (HR 0.65, 95% CI 0.58-0.72), and high genetic risk (HR 0.62, 95% CI 0.57-0.69, p < 0.001 for all). Overall, this study demonstrated that healthy lifestyle factors reduced the risk of developing gout in low, middle, and high genetic risk patients.
1. A mathematical model predicted that Individuals vaccinated for COVID-19 have lower infection rates when mixing strongly with other vaccinated individuals (10%), compared to mixing randomly with vaccinated and unvaccinated individuals (15%), as predicted by a mathematical model.
2. Unvaccinated individuals have higher infection rates when mixing strongly with other unvaccinated individuals (75%), known as like-with-like mixing, compared to mixing randomly with vaccinated and unvaccinated individuals (69%).
3. For the entire population, infection rates were highest with intermediate like-with-like mixing (27%), lower with random mixing (25%), and lowest with strong like-with-like mixing (24%).
Evidence Rating Level: 3 (Average)
The COVID-19 pandemic demonstrated not only rapid vaccine development, but widespread vaccine uptake as well. However, uptake is still considered suboptimal, which could have harms despite a population being predominantly vaccinated. To better illustrate these effects, this study created a mathematical model to exemplify potential interactions and mixing patterns between the vaccinated and unvaccinated. This model represented individuals as either susceptible to infection (S), infected and able to infect others (I), and recovered from infection and therefore immune (R), with individuals moving in the same order from S to I to R if coming into contact with I individuals. A certain percentage of the vaccinated population were considered immune in the model, depending on the effectiveness of the vaccine they took, with an 90% effective vaccine rendering 90% of individuals immune. As well, 20% of the unvaccinated were assumed to have baseline immunity from previous infection. Attack rates were calculated by the number of infections divided by the population size. This study included models of random mixing and like-with-like mixing, to account for how individuals may associate more with those of the same vaccination status. Overall, the study found that for the vaccinated, attack rates were higher at 15% in random mixing, compared to 10% with high like-with-like mixing. The reverse was true for the unvaccinated, with attack rates of 69% in random mixing, and 79% in high like-with-like mixing. For the entire population, the highest attack rates occurred with intermediate like-with-like mixing (27%), compared to random mixing (25%) and high like-with-like mixing (24%). In conclusion, this study showed that there are differences in infection rates depending on the extent to which the vaccinated and unvaccinated interact with each other, with strong like-with-like mixing or random mixing having lower infections amongst the general population than intermediate like-with-like mixing.
Image: PD
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.