2 Minute Medicine Rewind May 30, 2022
Self-selection vs Randomized Assignment of Treatment for Appendicitis
1. Patients with appendicitis who declined randomization of treatment and self-selected antibiotics, had similar rates of subsequent appendectomy at 30 days and 1 year, compared to those randomized to antibiotics.
Evidence Rating Level: 2 (Good)
Appendectomy and antibiotics are both common treatments for appendicitis. When comparing outcomes between the two, randomized controlled trials (RCTs) have demonstrated a lower percentage of appendectomy avoidance in patients randomized to antibiotics, when compared to observational cohort studies. This may be due to selection bias amongst patients who allow themselves to be randomized in RCTs, or it may be due to a self-fulfilling prophecy, where patients choosing a treatment they believe will work in observational cohorts leads to better outcomes. The current prospective study compared a cohort of RCT patients and a cohort of patients self-selecting their treatment, in order to determine differences in patient characteristics, quality-of-life outcomes, and rates of appendectomy amongst those receiving antibiotics. The study population consisted of 1094 patients in the RCT trial, and 510 patients declining randomization but joining the self-selected treatment cohort, from 25 medical centres in the United States. Individuals that had surgical contraindications, or severe appendicitis cases (such as involving septic shock or diffuse peritonitis) were excluded. The outcomes measured included severe adverse events, appendectomy among antibiotic patients, and the EuroQol Five-Dimension (EQ-5D) score 30-days post-discharge. In terms of patient characteristics, the study found that patients in the self-selection cohort were more frequently female (43% [95% CI 39-47%] vs 35% [95% CI 33-38%]), more college-educated (72% [95% CI 68-76%) vs 63% [95% CI 60-65%]), less frequently Spanish speakers (19% [95% CI 16-23%] vs 31% [95% CI 28-34%]), and more frequently had commercial insurance (53% [95% CI 48-57%] vs 45% [95% CI 42-48%]). In terms of patient outcomes, the EQ-5D scores at 30 days were similar between the two cohorts. In the self-selection antibiotics group, 15.3% underwent an appendectomy in 30 days (95% CI 10.7-19.7%) compared to 19.2% in the randomized antibiotics group (95% CI 15.9-22.5%). Therefore, the 30-day absolute difference was 3.9% (95% CI -1.7 to 9.5%), and at 1 year, it was 6.7% (9% CI -0.8 to 14.2%). Overall, this study showed that despite variation in patient characteristics, the outcomes between the RCT and self-selection cohorts were similar for appendectomy and antibiotic patients.
1. Childhood asthma has increased incidence among neighbourhoods with lower median household income, and among children with Black and Hispanic race.
2. Race and ethnicity remain as risk factors for increased childhood asthma incidence even after adjusting for neighbourhood income.
Evidence Rating Level: 3 (Fair)
Asthma is the most common chronic condition amongst children living in the United States, and is often preceded by wheezing in early childhood, from respiratory illnesses. Studies have shown that asthma disproportionately affects Black and Hispanic children, and that rates of asthma are higher in neighbourhoods with greater urbanicity and poverty. However, it is not currently known whether neighbourhood-level socioeconomic status mediates the relationship between race and ethnicity, and incidence of childhood wheezing and asthma. The current study examined this association for 5809 children (43,260 person-years) among 10 birth cohorts, from the Children’s Respiratory and Environmental Workgroup consortium. Metrics of neighbourhood socioeconomic status were collected from US census data, such as household income, population density, and percentage below poverty line. Individual data was also collected, including race and ethnicity, household income, and mother’s education level. The health outcomes assessed included incidence of asthma until 11 years of age, wheeze in early childhood (2 years of age or less), and persistent wheeze. The study found that there were significantly elevated incidences of asthma for Black (hazards ratio 1.47, 95% CI 1.26-1.73) and Hispanic children (HR 1.29, 95% CI 1.09-1.53), compared with White children, and the same was true for early and persistent wheeze. For higher median household neighbourhoods, there were lower incidences of asthma (HR 0.88, 95% CI 0.83-0.95), early wheeze, and persistent wheeze. However, there was no statistically significant interaction between race/ethnicity and neighbourhood socioeconomic status in the incidence of asthma: The incidence was still elevated for Black and Hispanic children in all census tracts, compared to White children. Overall, this study demonstrated that while neighbourhood income and race/ethnicity are important risk factors for childhood asthma, race/ethnicity remain as risk factors even after neighbourhood income was adjusted for.
1. Incidence of type 2 diabetes mellitus (T2DM) were similar among pre-diabetic adults treated with 3 years of eldecalcitol compared to placebo.
2. Amongst participants with the lowest basal insulin secretion, eldecalcitol significantly reduced the incidence of T2DM compared to placebo.
Evidence Rating Level: 1 (Excellent)
Vitamin D supplementation has been a proposed preventative strategy for type 2 diabetes mellitus (T2DM): Vitamin D is involved in insulin biosynthesis and secretion, and studies have found associations between low Vitamin D levels and higher incidence of T2DM. However, it is unknown if supplementation only benefits children with low Vitamin D. Therefore, the current randomized controlled trial compared the incidence of T2DM amongst adults with pre-diabetes, receiving either a placebo or the active vitamin D analogue eldecalcitol, for 3 years. The study population consisted of 626 patients receiving placebo and 630 patients receiving eldecalcitol, with a mean age of 61.3 (range 30-78) years. All patients were over 30 years old and had laboratory-confirmed impaired glucose tolerance. Additionally, 43.6% had Vitamin D deficiency at baseline, defined as concentrations <20 ng/mL, with the mean serum 25-hydroxyvitamin D concentration being 20.9 ng/mL. The study found that after a median follow-up of 2.9 years, there were no differences in incidence of T2DM, with 12.5% of the eldecalcitol group and 14.2% of the placebo group developing T2DM. The hazards ratio for eldecalcitol versus placebo was 0.87 (95% CI 0.67-1.17, p = 0.39). As well, 23.0% of the eldecalcitol and 20.1% of the placebo groups regressed to normoglycemia (HR 1.15, 95% CI 0.93-1.41, p = 0.21). However, after adjusting for covariates such as age, hypertension, family history of diabetes, vitamin D levels, and glucose tolerance lab values, the incidence of T2DM in the eldecalcitol group was deceased significantly (HR 0.69, 95% CI 0.51-0.95, p = 0.02). Furthermore, it was found that eldecalcitol reduced the incidence of T2DM for those in the lower third of HOMA-β, a biomarker for insulin secretion (HR 0.35, 95% CI 0.21-0.59, p<0.001), and HOMA-IR, a biomarker for insulin resistance (HR 0.37, 95% CI 0.20-0.67, p = 0.001), demonstrating that eldecalcitol benefitted individuals with lower basal insulin secretion. Overall, this study found no difference in T2DM incidence after treating pre-diabetic patients with eldecalcitol or placebo for 3 years, except for a lower incidence in the eldecalcitol group after adjusting for covariates, including lower basal insulin secretion.
1. Heavy goods vehicle (HGV) drivers participating in the 6-month Structured Health Intervention For Truckers (SHIFT) had improved physical activity outcomes after 6 months compared to a control group, with higher mean daily steps, less time spent sitting, more time standing, and more time engaging in moderate-to-vigorous physical activity.
2. Physical activity outcomes at 16-18 months were not different between the SHIFT cohort and the control group.
Evidence Rating Level: 1 (Excellent)
Heavy goods vehicle (HGV) drivers have high rates of obesity and associated chronic disease due to long hours of sedentariness, sleep deprivation, and poor dietary options. It has also been shown that HGV drivers have a higher rate of accidents compared to those in other occupations. The need for improved health promotion among HGV drivers spurred the development of the Structured Health Intervention for Truckers (SHIFT), a 6-month program that promotes physical activity and healthier dietary choices. The current randomized controlled trial compared physical activity outcomes at 6 months and 16-18 months, for HGV drivers participating in the SHIFT program, versus drivers carrying out their usual practice. The study population consisted of long-haul HGV drivers in the Midlands, UK, with 199 randomized to the control group and 183 randomized to the SHIFT program. Whereas the control group received educational pamphlets, SHIFT included a 6-hour education seminar on diet and exercise suggestions specific to their context as HGV drivers, provision of a Fitbit monitor, and continuous support and encouragement from coaches throughout the 6 months. The study found that at 6 months, the SHIFT cohort had significantly higher mean daily step counts (adjusted mean difference 1008 steps/day, 95% CI 145-1871, p = 0.022). The SHIFT group also had less time sitting (AMD -24, 95% CI -43 to -6, p = 0.011), more time standing (AMD 14, 95% CI 2-26, p = 0.024), and more time in moderate-to-vigorous physical activity (AMD 6, 95% CI 0.3-11, p = 0.038). However, these outcomes were not different between the groups after 16-18 months. Overall, this study demonstrated that there was increased physical activity at the end of the SHIFT program, but the long-term impact of the program after its conclusion is uncertain.
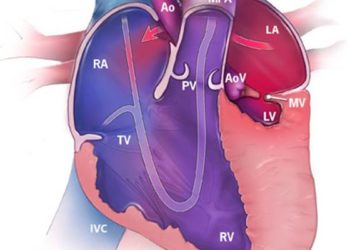
1. Compared to those not receiving early rhythm control (ERC), atrial fibrillation (AF) patients that receive rhythm control therapy within 1 year of diagnosis had a lower risk for stroke, and lower risk for a composite outcome of death from cardiovascular causes, stroke, and hospitalization for heart failure (HF) or myocardial infarction (MI).
2. AF patients receiving ERC did not have a lower risk for all-cause mortality, HF hospitalization, or MI hospitalization, compared to those not receiving ERC.
Evidence Rating Level: 2 (Good)
Patients with atrial fibrillation (AF) are at a higher risk of stroke and myocardial infarction (MI), and restoration of sinus rhythm has been shown to reduce mortality in observational studies. Past randomized controlled trials comparing rhythm control and rate control interventions have not shown a difference, with current guidelines recommending rate control first, and supplementing with rhythm control for symptom management if needed. However, the EAST-AFNET 4 trial demonstrated that for newly diagnosed AF patients, early rhythm control (ERC), which included AF ablation and continuation of anticoagulation therapy, significantly diminished risk for a composite end-point of cardiovascular-related death, stroke, worsening heart failure (HF) or acute coronary syndrome hospitalization. The current retrospective study aimed to examine the generalizability of these results, with a cohort of 79,948 patients diagnosed with AF during the enrollment period of EAST-AFNET 4. For analysis, these patients were divided into a control group, which did not receive rhythm control therapy within a year of diagnosis, and an ERC group, which included patients who received an antiarrhythmic drug (AAD) or AF ablation within a year. The study population had a mean±SD age of 71.0±11.6 years, 47.8% of whom were women, and 24.7% of whom received ERC. After a mean follow-up of 2.6±1.8 years, the results showed that ERC was associated with a decreased incidence of the composite outcome, with 9.45 compared to 11.13 events per 100 person-years (hazards ratio 0.85, 95% CI 0.75-0.97, p = 0.02). As well, ERC was associated with a diminished risk of stroke, with 1.10 compared to 1.70 events per 100 person-years (HR 0.66, 95% CI 0.47-0.93, p = 0.02). There was no significant reduction for all-cause mortality (HR 0.88, 95% CI 0.75-1.04, p = 0.14), HF hospitalization (HR 0.95, 95% CI 0.76-1.18, p = 0.61), or MI hospitalization (HR 0.76, 95% CI 0.54-1.08, p = 0.13). Overall, this study was concordant with the results of EAST-AFNET 4, with ERC patients having a decreased risk of the composite outcome.
Image: PD
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.