2 Minute Medicine Rewind November 11, 2024
Safety of simultaneous vs sequential mRNA COVID-19 and inactivated influenza vaccines
1. In this randomized clinical trial, the safety profile, including reactogenicity, was similar between the simultaneous or sequential administration of the quadrivalent inactivated influenza vaccine (IIV4) and COVID-19 vaccine.
2. This study supports the option of administering these vaccines simultaneously.
Evidence Rating Level: 1 (Excellent)
Getting vaccinated against influenza and COVID-19 have been associated with a decreased number of hospitalizations and deaths due to respective infections. According to the Centers for Disease Control and Prevention (CDC) it is recommended that these vaccines be given simultaneously at different anatomic sites. Due to a lack of evidence from previous studies, this study sought to provide further proof of the safety of the simultaneous vaccination recommendation. Individuals were deemed eligible to participate if they were 5 years or older getting the primary 2-dose vaccine series, or 12 years or older receiving a booster vaccine, and intended on receiving the COVID-19 vaccine and the influenza vaccine. Individuals were excluded if they were pregnant or planned on getting pregnant within the next 3 months, and immunosuppressed individuals. All participants gave a blood sample to determine their SARS-CoV-2 serostatus. On the first visit, the participants received the mRNA COVID-19 vaccine intramuscularly. Participants were randomized in a 1:1 ratio to either receive the FDA approved inactivated influenza vaccine (IIV4) or a saline placebo vaccine. During the second visit, the individuals previously administered the IIV4 vaccine received the placebo, and the placebo group received the IIV4 vaccine. Until day 121, the study assessed serious adverse events (SAEs) and adverse events of special interest (AESIs) along with corresponding medication change. Health-related quality of life (HRQOL) was assessed pre-vaccination and daily for 7 days. After primary assessment, 335 participants (mean [SD] age, 33.4 [15.1] years) received bivalent BNT162b2 mRNA COVID-19 vaccine. After randomizing the participants, 169 were assigned to the simultaneous group, and 166 to the sequential group. Compared to the simultaneous group, the proportion of participants in the sequential group [52 participants [31.3%]) that experienced the primary reactogenicity outcome was noninferior (43 participants [25.6%]) (site-adjusted difference, -5.6 percentage points [pp]; 95% CI, -15.2 to 4.0 pp). Between the simultaneous and sequential groups, there was no significant difference in the proportion of participants that had SAEs (1 [0.6%] vs 1 [0.6%] respectively; difference, -0.01 pp [95% CI, -1.66 to -1.64 pp]) ad AESIs (19 [11.2%] vs 9 [5.4%], respectively; difference, 5.8 pp [95% CI, -0.1 to 11.7 pp]). Overall, in this randomized clinical trial comparing simultaneous versus sequential administration of the COVID-19, and influenza vaccine, safety was comparable between the two methods.
Pressure-mediated biofeedback with pelvic floor muscle training for urinary incontinence
1. In this randomized clinical trial comparing the use of pelvic floor muscle training (PFMT) alone to PFMT with a biofeedback (BF) device, the use of PFMT with BF was superior in reducing stress urinary incontinence (SUI) in postpartum women.
Evidence Rating Level: 1 (Excellent)
Stress urinary incontinence (SUI) is a pelvic floor dysfunction disorder that has negative impacts on physical and mental health and thus quality of life. Many women experience SUI throughout their life, with the majority experiencing it for the first time during pregnancy or post-partum. The current first-line treatment recommendation for SUI is supervised pelvic floor muscle training (PFMT) for at least 3 months. However, physicians have wondered if there is an adjunct treatment that may provide additional benefits. So far, no method has gained acceptance. Thus, the goal of this study was to compare PFMT alone compared to PFMT with a home-based pressure-mediated biofeedback (BF) device, based on rates of improvement, PFM strength, and quality of life. Eligibility criteria included being aged 18 years or older, and clinically diagnosed with new-onset SUI in the 12 weeks post-delivery. Once deemed eligible, participants were randomized in a ratio of 1:1 to receive either PFMT with a home-based pressure-mediated BF device (intervention group), or PFMT alone (control group). To assess the primary outcome, urinary incontinence, the Chinese version of the International Consultation on Incontinence Questionnaire-Urinary Incontinence Short Form (ICIQ-UI SF) was used. A total of 452 participants (median age, 34 [IQR, 31-36] years; median time since delivery, 50 [IQR, 43-61] days) were split into the intervention group (n=223) and the control group (n=229). Compared to the scores at baseline, the ICIQ-UI SF score (representing severity) was significantly higher in the intervention group compared to the control group (3.00 [IQR, 1.00-6.00] vs 2.00 [IQR 0-4.00] points; z=-3.05; P=.002). Upon further comparison, the intervention group had a greater number of participants cured (45 of 223 [20.2%] vs 20 of 229 [8.7%]; z=12.02; P=.001) or improved (132 of 223 [59.2%] vs 102 of 229 [44.5%]; z=9.71; P=.002) than the control group. Both groups experience an increase in quality of life compared to baseline levels, but there was no significant difference between the groups. Overall, the results of this study show that PFMT and BF use was superior to PFMT alone in reducing SUI severity, and rates of cure in postpartum women.
1. In this prospective cohort of patients with acute myocardial infarction (AMI), plasma progranulin levels increased acutely after the AMI.
2. The increase in plasma progranulin levels in the acute phase after the AMI was associated with an improvement in cardiac function, specifically, an increase in left ventricle ejection fraction (LVEF) during the chronic phase.
Evidence Rating Level: 1 (excellent)
Progranulin is a secreted glycoprotein, regulates inflammation and wound healing, and is associated with frontotemporal dementia, and cancer. Previous studies have reported that the administration of progranulin reduces myocardial infarct size while also improving left ventricular function in rabbit models that had an acute myocardial infarction (AMI). The goal of this study was to investigate the relationship between left ventricle (LV) function 6 months after the onset of AMI. However, the role of plasma progranulin in the acute phase has yet to be thoroughly studied. Therefore, this prospective cohort study was conducted to determine the changes in progranulin levels in the acute phase after AMI, and the correlation with LV function in the chronic phase. Patients were included if they were admitted to Gifu Municipal Hospital due to anterior chest pain, underwent a coronary angiography, and were diagnosed with AMI based on extended chest pain, ST segment elevation, and an occluded coronary artery. Blood samples were taken from the participants from the antecubital vein to measure plasma progranulin levels. The participants also underwent echocardiography to measure left ventricular ejection fraction (LVEF), LV end-systolic dimension (LVSd), and LV end-diastolic dimension (LVDd). A total of 34 patients participated in the study, with 18 in the AMI group, and 16 in the control group. On day 0, there was no significant difference in plasma progranulin levels between the control group (69.5 ± 24.6 ng/mL) and the AMI group (84.2 ± 47.1 ng/mL. However, when measured on day 7, the progranulin levels were much higher in the AMI group (104.2 ± 52.0 ng/mL) compared to the control group (69.5 ± 24.6 ng/mL) (p=0.045). In patients with acute phase AMI, plasma progranulin levels increased significantly from 84.2 ± 47.1 ng/mL to 104.2 ± 52.0 ng/mL from day 0 to 7 respectively (P=0.0002). There was a positive association between the rise in plasma progranulin levels during the acute phase and the improvement in LVEF from the acute and chronic phase. This study was limited by the small number of patients with AMI, leading to reduced generalizability, and statistical power. Overall, in this retrospective cohort study of patients with AMI, plasma progranulin levels increased after AMI in the acute phase, and this increase was positively correlated with an increase in LVEF during the chronic phase.
1. In this pilot randomized controlled trial, the Sleep Mood Intervention: Life Effectively (SMILE) intervention was associated with improvements in insomnia in university students.
Evidence rating level: 1 (Excellent)
Insomnia has a major burden on public health and can have serious long-term physical and mental health effects if left untreated. A population at a high risk for sleep problems include university students which may be due to specific challenges that arise during this phase in life as balancing stress and developing greater independence. There is much research to support the use of cognitive behavioural therapy for insomnia (CBT-I), involving changing negative attitudes through the use of cognitive restructuring. In addition to CBT-I, mindfulness interventions, promoting being present in the moment, have promising results, specifically on reducing stress and anxiety. To study the effectiveness of mindfulness counselling on insomnia in university students, a randomized controlled trial created the Sleep Mood Intervention: Life Effectively (SMILE) intervention. The participants were assigned to the SMILE intervention group and a waiting list control group is a 2:1 ratio. The participants completed the Insomnia Severity Index (ISI) and those with a score of ≥ 10 were eligible for further screening including a face-to-face diagnostic interview using the M.I.N.I Plus International Neuropsychiatric Interview. Several inclusion criteria were listed including self-reported sleep complaints (ISI score ≥ 10), university enrollment, 18 years or older, English proficiency, and willing to participate in a 4-week program. After randomization, 23 people were assigned to the SMILE group and 12 were assigned to the waitlist group. Outcomes were assessed at baseline and after five weeks. Insomnia was assessed using the ISI, while depression was assessed using the Beck Depression Inventory II, and anxiety was assessed using the Hospital Anxiety and Depression Scale (HADS-A). The participants in the SMILE group had significantly lower severity levels of insomnia (M = 10.7, SD = 4.8) compared to the waitlist group (M = 14.7, SD = 4.9), post-test (t (33) = 2.33; p = .03, [95% CI: 0.51 to 7.52]. The impact of the SMILE intervention effects on insomnia severity was mediated by dysfunctional beliefs, with a reduction in dysfunctional beliefs associated with a decrease in insomnia severity, b = 1.12, [95% CI: -2.58 to -0.06]. There were no significant effects found for depression, d = 0.02 [95% CI: -0.35 tp 0.37], anxiety, d = 0.15 [95% CI: -0.16 to 0.53] and quality of life, d = 0.09 [95% CI: -0.25 to 0.42]. Overall, university students struggling with insomnia experienced improvements in their symptoms after participating in the four-week SMILE intervention.
1. In this retrospective cohort of patients with atrial fibrillation (AF) who underwent transcatheter aortic valve replacement (TAVR), the patients with a higher direct oral anticoagulants (DOAC) Score, had a higher bleeding risk.
Evidence Rating Level: 2 (Good)
Atrial fibrillation (AF) is increasingly seen in the aging population and is associated with severe adverse health outcomes such as stroke or death. Thus, immediate and appropriate management is crucial to preventing these health outcomes. Oral anticoagulants (OACs) have been prescribed to patients with AF to manage outcomes. Specifically, direct oral anticoagulants (DOACs) are the preferred type due to their strong effectiveness in preventing strokes while limiting bleeding. The goal of this study was to evaluate the association between the DOAC Score and bleeding events in patients with AF after undergoing transcatheter aortic valve replacement (TAVR). This retrospective cohort study included patients with a diagnosis of AF from electrocardiogram. Patients were excluded if they had missing data, death within the hospital after TAVR, or were not on OAC treatment. Vitamin K antagonists (VKAs) doses were prescribed to maintain prothrombin time in the patients. Based on their DOAC score, patients were divided into 3 groups. These included the low and moderate-risk group (DOAC Score ≤7), high-risk group (DOAC Score 8-9 points) and very high-risk group (DOAC Score ≥ 10 points). There were 380 (30.1%) patients in the low and moderate-risk group, 497 (40.4%) in the high-risk group, and 353 (28.7%) patients in the very high-risk group. After meeting the eligibility criteria this study included 1230 patients (mean age, 84.6±5.1 years, 37.2% men). Of these patients, 465 (37.8%) received a VKA, while the rest received DOACs. Comparing the between-group results, 23 patients (6.1%), 34 patients (6.8%) and 50 (14.2%) of patients in the low and moderate-risk group, high-risk group, and very high-risk group, respectively, had bleeding events occur. These groups also had significant differences in the 3-year cumulative incidence of all bleeding events. The low and moderate risk group had a 6.6% incidence, the high-risk group had a 6.9% incidence, and the very high-risk group had a 14.0% incidence (P<0.01). The 3-year cumulative incidence was also measured for the DOAC and VKA cohorts and was significantly different. The incidence was 5.5%, 6.7%, and 12.3% respectively, in the DOAC cohort (P=0.002), and 8.8%, 7.4%, and 16.0%, respectively, in the VKA cohort (P=0.04). When the DOAC score increased, there was a significantly higher incidence of bleeding events in all cohorts (HR, 1.22 [95% CI, 1.08-1.38]; P<0.01 for the overall population; HR, 1.20 [95% CI, 1.01-1.42]; P=0.04 for the DOAC cohort; and HR, 1.25 [95% CI, 1.04-1.50]; P=0.02 for the VKA cohort). Overall, there was a significant association between the DOAC score and risk of bleeding after TAVR in patients with AF. The DOAC score could be useful in future research in predicting bleeding risk in patients receiving OACs.
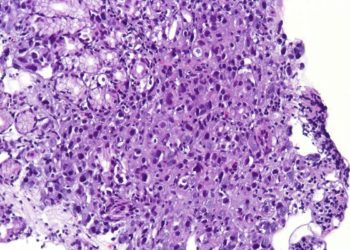
Image: PD
©2024 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.