2 Minute Medicine Rewind November 20, 2023
1. This randomized clinical trial found that over a 26-week period, both accupuncture and massage effectively reduced pain and improved fatigue, insomnia, and quality of life among patients living with advanced cancer.
2. There was no significant difference between acupuncture or massage for measured outcomes.
Evidence Rating Level: 1 (Excellent)
Pain affects up to two-thirds of patients with advanced cancer. While oncologic pain has historically been managed with drug therapies, amid the ongoing opioid crisis, non-pharmacologic alternatives are being explored. The 2022 joint guideline by the American Society of Clinical Oncology and Society for Integrative Oncology recommends acupuncture and massage, but there is a paucity of literature among patients with advanced cancer. The Integrative Medicine for Pain in Patients with Advanced Cancer Trial (IMPACT) is a pragmatic, 2-arm, parallel-group randomized clinical trial, aimed at comparing the long-term effectiveness of acupuncture and massage in managing pain, along with comorbid fatigue and insomnia in advanced cancer patients. 300 patients (mean [SD] age, 68.7 [14.1] years; 67.1% women) with an advanced cancer diagnosis were randomized in a 1:1 ratio to receive acupuncture or massage. From baseline to week 26, acupuncture demonstrated a mean reduction of -2.53 points (95% CI, -2.92 to -2.15) in the BPI worst pain score, a reliable, valid, and responsive measure of pain. Massage exhibited a mean change of -3.01 points (95% CI, -3.38 to -2.63). However, the between-group difference in BPI worst pain reduction was not statistically significant. By week 26, over half of the patients demonstrated a clinical response to treatment (defined as 30% improvement from baseline), with 55.2% (95% CI, 46.0%-64.0%) for acupuncture and 65.9% (95% CI, 57%-74%) for massage. At week 26 compared to baseline, both acupuncture and massage exhibited reduced analgesic medication use and enhancements in pain-related functional interference, fatigue, insomnia and physical quality of life. Overall, these findings suggest that while there was no significant difference between treatments, both acupuncture and massage effectively reduce pain and improve fatigue, insomnia, and quality of life among patients living with advanced cancer.
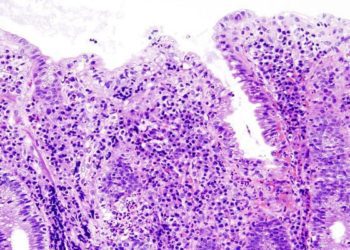
1. In this secondary analysis of the Optimal Antiplatelet Therapy for Prevention of Gastrointestinal Injury Evaluated by ANKON Magnetically Controlled Capsule Endoscopy (OPT-PEACE) tria, continuous administration of aspirin, clopidogrel, or their combination from 6 to 12 months post-PCI led to notable progression of gastric and small-intestinal injury, particularly with dual antiplatelet therapy compared to monotherapy.
Evidence Rating Level: 1 (Excellent)
Antiplatelet therapy is crucial for secondary prevention in cardiovascular disease after PCI. While guidelines recommend clopidogrel plus aspirin for at least 12 months post-PCI, antiplatelet agents increase the risk of gastrointestinal bleeding (GIB). This secondary analysis of the OPT-PEACE trial—a double-masked, placebo-controlled, multicenter randomized clinical trial conducted at 28 centers in China—aims to evaluate the association of aspirin, clopidogrel, and dual antiplatelet therapy (DAPT) with gastrointestinal injury progression among patients without high bleeding risk after PCI using serial magnetically controlled capsule endoscopy (MCE). 394 patients (mean [SD] age, 56.9 [8.7] years; 75.1% men) who received 6-months of DAPT were randomized in a 1:1:1 ratio to receive aspirin alone (n = 132), clopidogrel alone (n = 132), or DAPT (n = 130). MCEs were performed at baseline, after the initial 6-months of DAPT, and 6-months after randomization (12-months post PCI). Between MCEs at 6 and 12 months, gastric injury occured in 37.1% of aspirin users, 48.5% of clopidogrel users, and 53.1% of DAPT users (P=0.02), with a significantly lower progression in aspirin users compared to DAPT (RR, 0.70 [95% CI, 0.49-0.99]; P = .009). Small-intestinal injury during the same period occurred in 38.6% of aspirin users, 49.2% of clopidogrel users, and 54.6% of DAPT users (P = .03), again with a lower rate of small-intestinal injury progression in aspirin users compared to DAPT (RR, 0.71 [95% CI, 0.50-0.99]; P = .01). For both gastric and small-intestinal injuries, no significant differences were noted in injury progression between clopidogrel alone and DAPT, or between aspirin alone and clopiogrel alone. All previous findings remained consistent in subgroup analysis of patients with pre-existing injury from the initial 6 months of DAPT. Overall, these findings suggest that among patients without high bleeding risk who received a 6-month DAPT course after PCI, aspirin, clopidogrel, and their combination were all associated with gastrointestinal injury progression in a susbtantial portion of patients. Aspirin monotherapy had the lowest rate of progressive gastrointestinal injury among the 3 regimens.
1. This randomised control trial demonstrated that a standardised and manualised intervention in primary care showed a sustained reduction in lower urinary tract symptoms (LUTS) in men at 12 months, as assessed through the International Prostate Symptom Score (IPSS).
2. The mean IPSS difference between the intervention and control arm of −1.81 points, while statistically significant, was less than the predefined target reduction of 2.0 points.
Evidence Rating Level:1 (Excellent)
LUTS, encompassing issues with urine storage and voiding, affect around 30% of men aged 65 and older, significantly impacting their quality of life. Guidelines recommend using conservative treatments for LUTS initially, such as bladder training, fluid intake advice, and lifestyle guidance. However, inconsistent provision for LUTS in men in primary care underscores the need for practical resources to support symptom assessment and boost patient engagement in conservative management. The Treating Urinary Symptoms in Men in Primary Healthcare (TRIUMPH) study—a multicentre, pragmatic, two arm cluster randomised controlled trial in UK primary care—aims to asess whether a standardised and manualised care intervention could yield superior improvement of LUTS in men compared with usual care. 33 primary care sites were randomized in a 1:1 ratio to administer the intervention or usual care. The intervention included a standardised information booklet that provides guidance on conservative and lifestyle interventions for LUTS in men. Patients were directed to applicable information in the booklet after professional healthcare assessment and discussion, providing the manualised element of the intervention. 524 participants were recruited from intervention sites and 553 from usual care sites. At 6 and 12 months, both arms showed improvement in LUTS, with a greater reduction in the intervention arm (IPPS difference 6 months, −1.68 (−2.34 to −1.02); 12 months, <0.001; IPSS difference -1.81; 95% CI -2.66 to -0.95; P<0.001). The observed reductions were less than the predefined target reduction of 2.0 points, indicating that the improvement in symptoms associated with the intervention may be modest. With regards to secondary outcomes, incontinence scores, mean IPSS LUTS specific quality of life scores, and patient perception of their LUTS, demonstrated greater improvement in the intervention arm compared to the usual care arm at both 6 and 12 months. Overall, these findings suggest that a standardised and manualised intervention achieved a small, statistically significant, sustained reduction in LUTS.
1. In this randomized controlled trial of patients with patellofemoral pain (PFP), home-based exercise resulted in less pain, better function, and higher knee muscle strength compared with no exercise.
Evidence Rating Level: 1 (Excellent)
PFP, a common knee disorder characterized by diffuse retropatellar pain, affects many aspects of daily life in both athletic and nonathletic populations. Exercise therapy, especially hip and knee-targeted programs, is beneficial in managing PFP. Home-based programs have gained significance, particularly during the COVID-19 pandemic. This randomized controlled trial conducted between March and October 2022 aims to evaluate the efficacy of a six-week home-based program’s impact on pain, knee function, and muscle strength in PFP patients. 38 patients with PFP were recruited and randomized in a 1:1 ratio to the intervention (home-based exercise with health education) or control group (included only patient health education but no exercise). At 6 weeks, the intervention group experienced significant improvements in pain intensities for worst pain and pain with activities of daily living (ADL) from baseline (% improvement 42% and 52%, respectively; P < 0.01), while the control group only showed significant improvement in worst pain (4%, P = 0.02). When comparing groups, delta analysis revealed significantly greater improvements in the intervention group for both measures (P < 0.01). With regards to the Anterior Knee Pain Scale (AKPS), a 13-item self-report questionnaire that assesses mobility capacity across six activities and related symptoms of PFP, there was a significant improvement in AKPS from baseline in the intervention group (15%, P < 0.01), while the control group showed no significant change. The between-group difference was statistically significant with a P-value of <0.01 favouring the intervention group. Over six weeks, the intervention group significantly improved knee extensor strength (11%, P < 0.01), while knee flexor strength showed no significant change (P = 0.68). The control group demonstrated no strength improvements. The intervention group demonstrated superior improvement in knee extensor strength (P < 0.01) compared to the control group, when comparing groups. Overall, these findings suggest that a six-week home-based exercise and health education program significantly improved pain intensity, function, and knee extensor strength compared with no exercise for patients with PFP.
1. This randomized pilot study demonstrates that fasting blood glucose (FBG), systolic blood pressure (SBP), diastolic blood pressure (DBP), body mass index (BMI), and body fat percentage (BFP) were significantly improved with aerobic training, strength training, or combined aerobic plus strength training, compared with the control group in patients with T2DM.
2. The combined exercise intervention was the most successful in altering these parameters.
Evidence Rating Level: 1 (Excellent)
Diabetes mellitus affects 382 million adults globally, projected to increase to 439 million by 2030, with 85–95% being T2DM. A sedentary lifestyle is a major risk factor for T2DM and its complications, making physical activity a vital non-pharmacological treatment. This pilot trial assesses various exercise modalities (aerobic, resistance, and combined) against a control group, aiming to compare their effectiveness in the improvement of blood glucose, blood pressure, and body composition among T2DM patients. 40 participants were recruited and randomly assigned to the aerobic training group (ATG: n = 10), resistance training group (RTG: n = 10), combined training group (resistance plus aerobic; CTG: n = 10), and control group (CG: n = 10). All intervention groups experienced significant (P<0.005) improvements in FBG (mean difference, -13.03; p < 0.001), SBP (21.63 mmHg; p < 0.001) , DBP (11.86 mmHg; p < 0.001) and (BFP 9.14; p < 0.001) from pre- to post-test, but there was no significance differences in control group. ANCOVA with a Post hoc test was used to determine which training intervention had the greatest impact relative to the control group. All three interventions demonstrated significant differences compared with the control group for FBG, SBP, DBP, BMI and BFP (p < 0.001). Generally, combined training more significantly reduced BMI, FBG, SBP, DBP and BFP compared to the control group. These results remained consistent after controlling for diet, gender, and age, suggesting that the observed benefits were primarily attributable to the exercise interventions. Overall, these findings demonstrate regular physical exercise positively affects blood glucose control, blood pressure, and body composition in patients with T2DM, with combined aerobic plus resistance exercise emerging as the most effective in enhancing these parameters.
Image: PD
©2023 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.