2 Minute Medicine Rewind November 4, 2024
1. Suboptimal carbohydrate consumption is negatively associated with male fertility but not female fertility
Evidence Rating Level: 3 (Average)
Subfertility is the inability to conceive after 12 months of unprotected intercourse and affects millions of couples globally. Many factors such as age and genetics are non-modifiable, however diet has become the focus of modifiable factors influencing fertility. High glucose levels affect insulin sensitivity, hormonal balance, and ovarian function. Hyperglycemia can also cause oxidative stress which can contribute to subfertility. The glycemic index (GI) and glycemic load (GL) are dietary measures that assess carbohydrate quality and intake. High GL or GI diets have been suggested to affect fertility in women and possibly males as well. This prospective cohort study explored associations of periconception dietary GI and GL with subfertility. Dietary information was collected using a questionnaire. The time to pregnancy was also assessed using questionnaires during the preconception period and early pregnancy. Higher dietary GI and GL in women was not associated with fecundability however for men, higher GI and GL was associated with decreased fecundability. This association remained after adjusting for socio-demographic and lifestyle factors, as well as dietary GI or GL of female partners. There was no significant association between the dietary GI and GL in quartiles with fecundability in either women or men. Similarly, low Gi diets showed no significant effect on fecundability or risk of subfertility in men or women.
1. 72-hour delayed serum sample processing had no effect on testing for cytokines, chemokines, cfDNA, or coagulation in healthy volunteers and ICU patients
Evidence Rating Level: 2 (Good)
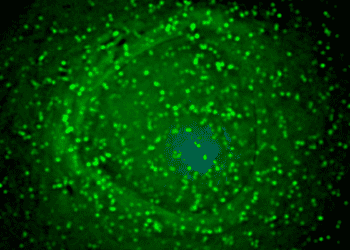
Plasma and serum markers are routinely collected for critically ill patients. Community hospitals, which care for the majority of Canadian patients, do not have the infrastructure to process and store these samples. A central site for processing has been suggested to allow community hospitals to conduct studies faster. However, the effect of delayed sample processing on serum markers, blood clotting factors, and other tests is unclear. This study aimed to determine the effect of delayed blood processing of up to 72 hours on the stability of plasma biomarkers commonly studied in critically ill patients. Participants had blood drawn into three citrate tubes and one EDTA tube. Aliquoted blood was kept at various re-processing conditions: RT vs 4˚C, and 0-, 24-, 48-, or 72-hours pre-processing delay. Delayed processing did not significantly affect levels of IL-6, IL-10, TNF, or IFN-γ (ANOVA, p = 0.31, p = 0.08, p = 0.30, p = 0.32, respectively). No significant changes in IL-6 levels were observed in citrate or EDTA samples from healthy volunteers (ANOVA p = 0.67 at RT and p = 0.35 at 4˚C) (S1 Fig) or ICU patients (ANOVA p = 0.55 at RT and p = 0.63 at 4˚C). Similarly, temperature did not affect IL-6 levels. No changes were seen in the tested chemokines either: IL-8, IP-10, MCP-1, MCP-4, MIP-1α, or MIP-1β (ANOVA, p = 0.31, p = 0.21, p = 0.36, p = 0.06, p = 0.57, and p = 0.35, respectively). To test cell death, cfDNA was examined. No changes were found after delayed processing in either temperature for both ICU and healthy participants (ANOVA p = 0.89 and p = 0.46, respectively). Finally, no changes were seen in coagulation studies including lag time and total thrombin formation. Therefore, delayed sample processing is a viable solution for conducting biosampling in community hospitals.
1. Hydroxychloroquine significantly improves the lipid profile in patients with rheumatoid arthritis and systemic lupus erythematosus
Evidence Rating Level: 1 (Excellent)
Patients with rheumatoid arthritis (RA) and systemic lupus erythematosus (SLE) have an increased morbidity and mortality from cardiovascular disease (CVD) due to the inflammatory nature of these conditions. Several observational studies have shown a reduction in in CVD risk in these patients if treated with hydroxychloroquine (HCQ). This interventional study was done to evaluate the effect of HCQ treatment on the CVD risk factors (blood lipids, glucose metabolism, and blood pressure) in patients with RA or SLE. Four weeks after the initiation of HCQ, total cholesterol, LDL, and ApoB levels were significantly reduced. HDL, triglycerides, ApoA1 and Lp(a) levels did not change significantly. HbA1c decreased in most patients with greater changes seen in those with higher initial HbA1c (correlation coefficient -0.77, p<0.0001). Vascular function analysis done with Arteriograph® showed no significant changes in pulse-wave velocity, aortic or brachial augmentation index, aortic blood pressure or pulse pressure during the 8-week treatment with HCQ. These results suggest that HCQ treatment in patients with RA and SLE shows a significant improvement of lipid status and decreased HbA1c. The main limitation is the sample size which included 25 patients with RA and 7 with SLE. Future studies should validate this with larger cohorts.
MRI-Based Prediction of Macrovascular Causes of Intracerebral Hemorrhage
1. The MRI Assessment of the Causes of intRacerebral haemOrrhage (MACRO) score shows greater predictive accuracy than existing CT-based scores for determining etiology of spontaneous intracerebral hemorrhage
Evidence Rating Level: 2 (Good)
Non-traumatic, spontaneous intracerebral hemorrhage (ICH) accounts for 10-30% of all strokes but accounts for half of the disability-adjusted life years lost due to strokes globally. These strokes are subdivided into small vessel diseases and macrovascular causes. The etiology influence treatment and prognosis. CT angiography (CTA) is the first-line investigation to identify macrovascular causes. Digital subtraction angiography (DSA) is a highly invasive procedure with significant risk of complications including hematoma and cerebral ischemia but remains the reference standard investigation. Therefore, a clinical score to select patients to undergo DSA is necessary. This study aimed to develop such a score using data from 2 large cohort studies. ICH patients who had a brain MRI and angiography within 90 days of symptom onset were included. Lasso logistic regression was used to create the score. The MRI Assessment of the Causes of intRacerebral haemOrrhage (MACRO) score includes age (0–39, 40–69, or ≥70), location of ICH (lobar, deep, or infratentorial), and SVD markers on MRI (≥1 microbleed, ≥1 lacune, presence of cortical superficial siderosis, or white matter hyperintensities using the Fazekas scale). Compared to existing CT-based scores, the MACRO score showed superior predictive ability (p < 0.001).
1. Higher CEA levels in patients with colorectal cancer are indicative of aggressive tumour phenotypes and survival
Evidence Rating Level: 2 (Good)
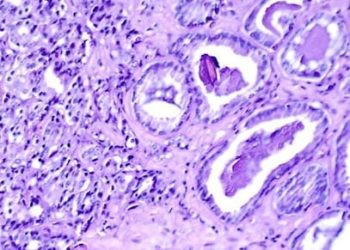
Despite progress in early screening and treatment for colorectal cancer (CRC), prognosis has not improved with a 5-year survival rate around 60%. Identifying reliable prognostic factors is crucial for guiding clinical decisions and can improve the prognosis of patients. Prognosis of CRC is influenced by TNM staging and various pathological factors including microsatellite instability, histological type, and differentiation amongst others. To bypass the invasive nature of these tests, serum biomarkers such as carcinoembryonic antigen (CEA) are being investigated as a prognostic factor as it is significantly elevated in cancer patients. This study aimed to create a CEA grading system for CRC patients. Patients with pathologically confirmed CRC with complete pre and postoperative data and serological testing were included. CEA levels were normal in 57.3% of patients, mildly elevated in 25.6%, moderately elevated in 9.1% and severely elevated in 8.0%. The median CEA in these patients was 3.95. Patients with CRC recurrence had an elevated CEA of 6.62 with the non-recurrence group having a CEA of 3.48. Similarly, CEA was higher in patients that died (5.98) relative to those who did not (3.18). A Kaplan-Meier survival analysis showed CEA levels could be used to stratify patients with CRC. The prognosis showed a stepwise decline as CEA increased in both progression-free survival (67.8% vs 55.1% vs 46.5% vs 32.1%, p<0.001) and overall survival (70.1% vs 56.6% vs 46.5% vs 34.0%, p<0.001). CEA grading could also stratify patients into the same stages as TNM staging. Higher CEA levels were also associated with more aggressive tumour phenotypes.
Image: PD
©2024 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.