2 Minute Medicine Rewind November 4-10, 2013
Image: PD
In this section, we will highlight the key high-impact studies, updates, and analyses published in medicine during the past week.
Dolutegravir Plus Abacavir-Lamivudine for the Treatment of HIV-1 Infection
Antiretroviral therapy in the treatment of human immunodeficiency virus (HIV) infection has dramatically improved the survival of HIV-positive patients, but traditional therapy is far from perfect. In this randomized, double-blind, phase 3 trial, 844 previously untreated HIV-positive patients were randomized to treatment with dolutegravir-abacavir-lamivudine or the currently recommended combination therapy (efavirenz-tenofovir disoproxil fumarate-emtricitabine) with a primary outcome of proportion of participants with an undetectable viral load at 48 weeks. Viral suppression was achieved in 88% of the treatment group compared to 81% of those in the control group (p=0.0003). The dolutegravir group also had a shorter median time to viral suppression (28 vs 84 days, p<0.001), greater increase in CD4 T-cell count (difference of 59 cells/mm3, 95% CI 33-84, p<0.001), and fewer reported significant or life-threatening adverse events (10% vs 16%).
Millions of outpatient visits each year for pharyngitis contribute to crowded clinics and patient frustration when no testing or treatment is recommended based on history and physical exam. Researchers analyzed a cohort of 71,776 visits to MinuteClinic urgent care centers in 9 areas of the United States in order to develop a “home score” tool that may be used by patients in deciding whether or not to see a physician at all. The home score is based only on the history (age, fever, absence of cough) and the recent local proportion positive (RLPP) – a biosurveillance marker for local prevalence of the disease in the past 14 days. At a threshold score of <10, the home score had a sensitivity of 99% and a negative predictive value of 0.9. This was comparable to existing models, the Centor and McIsaac scores, which take into account both history and physical exam characteristics (sensitivities of 80% and 75% and negative predictive values of 0.88 and 0.87, respectively). Investigators postulate that if applied nationally, the home score model could result in 230,000 fewer visits annually while missing an additional 8500 cases of GAS compared to a Centor score-based model.
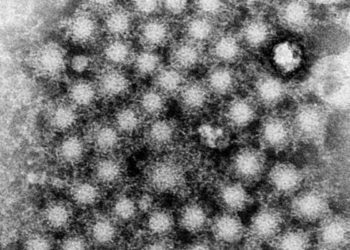
Interferon-based therapy has been the standard in treating Hepatitis C virus (HCV) infection, but is not suitable for many patients due to adverse events or contraindications such as psychiatric illness. In this randomized trial, 100 patients with HCV, divided into cohort A (treatment-naïve) and B (previously failed protease inhibitor treatment), were randomized to various interferon-free regimens to study the effect on sustained virological response 12 weeks after treatment (SVR12). Cohort A patients were randomized to receive sofosbuvir + ledipasvir for 8 weeks; sofosbuvir + ledipasvir and ribavirin for 8 weeks; or sofosbuvir + ledipasvir for 12 weeks. Cohort B was randomized to receive sofosbuvir + ledipasvir for 12 weeks or sofosbuvir + ledipasvir and ribavirin for 12 weeks. All participants had rapid reductions in serum HCV RNA, and none had virological breakthrough during treatment. Ninety-seven percent of patients achieved SVR12 and SVR at 24 weeks, irrespective of prior treatment history, disease severity, presence or absence or ribavirin in the treatment regimen, or race. The treatments were not without adverse events, but no patients discontinued treatment because of an adverse event.
Calcium-Channel Blocker – Clarithromycin Drug Interactions and Acute Kidney Injury
Calcium-channel blockers such as amlodipine, nifedipine, and verapamil are metabolized by the cytochrome P450 3A4 enzyme (CYP3A4). Prior case reports and studies have implicated concurrent administration of calcium channel blockers with a CYP3A4 inhibitor such as erythromycin or clarithromycin in hypotension requiring hospitalization. Acute kidney injury (AKI) is a clinically important consequence of hypotension. In this retrospective cohort study, researchers compared the risk of hospitalization for AKI in 190,000 Canadian patients over 65 who were prescribed both a calcium-channel blocker and either clarithromycin, a CYP3A4 inhibitor, or azithromycin. There was a small but statistically significant increase in AKI in patients who received clarithromycin compared to azithromycin (0.44% vs 0.22%, adjusted OR 2.03, 95% CI 1.72-2.41). All-cause mortality was also higher in those who received clarithromycin (adjusted OR 1.74, 95% CI 1.57-1.94). Co-prescribing calcium-channel blockers and CYP3A4 inhibitors such as clarithromycin is common and may result in easily avoidable hospitalizations and costs to the health care system.
Lack of sleep has been well-established to impair performance in many situations, including in providing medical care. However, prior studies, limited by small sample sizes, found no association between sleep deprivation and attending surgeons’ performance or patient outcomes the day after. In this retrospective cohort study, investigators matched each of 2078 Canadian patients who underwent laparoscopic cholecystectomies by surgeons who had operated between midnight and 7am the night before, to 4 other elective laparoscopic cholecystectomies performed by the same surgeon (n=8312). The primary outcome was conversion to an open cholecystectomy, and researchers found no significant difference between the 2 groups (2.2% vs 1.9% of those who had not operated the night before, adjusted OR 1.18, p=0.33). Similarly, there was no difference in the risk of iatrogenic injuries (OR 0.77, p=0.37) or death (OR not reported, p=0.57). This contradicts safety concerns relating to surgeons operating under sleep deprivation, though it does not take into account possible communication errors or cancelled procedures due to surgeon fatigue.
By Kathleen Li and David Ouyang
© 2013 2minutemedicine.com. All rights reserved. No works may be reproduced without written consent from 2minutemedicine.com. Disclaimer: We present factual information directly from peer reviewed medical journals. No post should be construed as medical advice and is not intended as such by the authors or by 2minutemedicine.com. PLEASE SEE A HEALTHCARE PROVIDER IN YOUR AREA IF YOU SEEK MEDICAL ADVICE OF ANY SORT. Content is produced in accordance with fair use copyrights solely and strictly for the purpose of teaching, news and criticism. No benefit, monetary or otherwise, is realized by any participants or the owner of this domain.