2 Minute Medicine Rewind November 7, 2016
Coronary artery bypass grafting (CABG) is the standard treatment for revascularization in patients with left main coronary artery disease. However, percutaneous coronary intervention (PCI) is being increasingly performed for this indication. In this multicenter randomized controlled trial, 1201 patients with stable or unstable angina pectoris or acute coronary syndrome with left main stenosis were randomized to undergo CABG or PCI with a drug-eluting stent to determine whether PCI is non-inferior to CABG in the treatment of left main coronary artery disease. The primary endpoint of this study was major adverse cardiac or cerebrovascular events (MACCE). Based on Kaplan-Meier estimates of MACCE, researchers found that 29% of patients from the PCI group were expected to experience MACCE after 5 years of follow-up, compared to 19% of patients that underwent CABG (HR 1.48, 95% CI 1.11 to 1.96, p=0.0066). Specifically, patients that underwent PCI conferred a significantly higher risk of experiencing non-procedural myocardial infarction (HR 2.88, 95% CI 1.40 to 5.90, p=0.0040), requiring revascularization (HR 1.50, 95% CI 1.04 to 2.17, p=0.032), revascularization with CABG (HR 9.40, 95% CI 2.19 to 40.38, p=0.0026) and de-novo lesion revascularization (HR 2.34, 95% CI 1.16 to 4.74, p=0.018). This study therefore shows that CABG may provide superior clinical outcomes in the treatment of left main coronary artery disease compared to PCI.
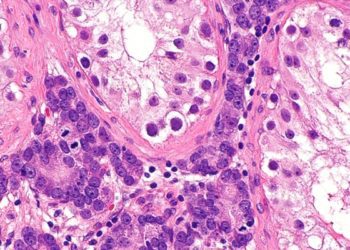
Vasectomy and risk of prostate cancer: population-based matched cohort study
Some studies have indicated that vasectomy may be associated with an increased risk of prostate cancer. However, these studies have been limited by small sample sizes, possible selection, recall and detection biases. In this population-based cohort study, 326,607 men that had undergone vasectomy were identified using large healthcare databases and followed up to characterize the association between vasectomy and prostate cancer, adjusting for measure of health-seeking behaviour. Each man that underwent vasectomy was matched to a control, based on age, comorbidity score, geographic area and index date. Without adjusting for other variables, researchers found that the incidence of prostate cancer in the vasectomy group, 53.2%, exceeded that observed in the non-vasectomy group, 46.8% (HR 1.13, 95% CI 1.05 to 1.20). However, upon performing a multivariate analysis, the association between vasectomy and incident prostate cancer was no longer significant (HR 1.02, 95% CI 0.95 to 1.09). In conducting sensitivity analyses, the authors also found no statistically significant difference after restricting to men with follow-up up to at least age 50 (HR 1.06, 95% CI 0.98 to 1.15) or at least age 60 (HR 1.06, 95% CI 0.91 to 1.23). Vasectomy was also not associated with advanced stage at diagnosis, prostate-cancer specific mortality, or incident non-Hodgkin’s lymphoma. This study therefore shows that vasectomy is not associated with incident prostate cancer.
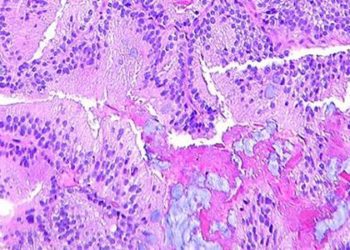
Benefits and risks of antiretroviral therapy for perinatal HIV prevention
Although there are clear benefits to the use of combination antiretroviral therapy (ART) regimens for the prevention of mother-to-child of human immunodeficiency virus (HIV) transmission, there are also risks. Specifically, studies have shown higher rates of adverse pregnancy outcomes with maternal ART compared to regimens containing fewer antiretroviral agents. In this randomized controlled trial, 3490 HIV-infected women at 14 or more weeks of gestation were randomized to 1) receive zidovudine and single-dose nevirapine plus a 1-2 week post-partum “tail” of tenofovir and emtricitabine (zidovudine alone), 2) zidovudine, lamivudine, and lopinavir-ritonavir (zidovudine-based ART), or 3) tenofovir, emtricitabine, and lopinavir-ritonavir (tenofovir-based ART) to evaluate the efficacy and safety of these regimens in preventing mother-to-child transmission during pregnancy among asymptomatic HIV-infected pregnant women with high CD4 counts. Researchers found that the rate of transmission was significantly in the ART groups (0.5%) was significantly lower compared to the group that received zidovudine alone (1.8%), corresponding to a difference of -1.3% (95% CI -2.1% to -0.4%). However, the rate of maternal grade 2-4 adverse events was significantly higher with zidovudine-based ART compared to zidovudine alone (21.1% vs. 17.3%, p=0.008. With respect to adverse pregnancy-related outcomes, the authors found that there was no significant difference between the ART groups (p>0.99). However, compared to the zidovudine-only group, a birth weight of less than 2500g was more frequent in the zidovudine-based ART (23.0% vs. 12.0%, p<0.001) and tenofovir-based ART (16.9% vs. 8.9%, p=0.004) groups. Furthermore, tenofovir-based ART was associated with higher rates of very preterm delivery (<34 weeks) compared to zidovudine-based ART (6.0% vs. 2.6%, p=0.04) and early infant death (4.4% vs. 0.6%, p=0.001). The rate of HIV-free survival was highest among infants whose mothers received zidovudine-based ART. This study therefore shows that while antenatal ART results in a significantly lower rate of early HIV transmission than zidovudine alone, it also confers a higher risk of adverse maternal and neonatal outcomes.
Advance care planning (ACP) is an iterative process involving discussions surrounding a patient’s preferences for end-of-life care, the completion of advance care directives and the designation of substitution decision makers. While ACP has increased over time, there is concern that certain patient populations, including minorities and those with lower levels of educational attainment, are not receiving the same quality of care as that seen among patients of a higher socioeconomic status. In this cross-sectional study, 2015 patients from a nationally representative sample of community-dwelling Medicare beneficiaries age 65 years and older were asked to report on whether they had engaged in ACP discussions. Specifically, participants were asked if they had 1) discussed with any individual the medical treatment desired if seriously ill in the future, 2) had legal arrangements for a proxy to make decisions about medical care, and 3) had written instructions about medical treatment desired. Researchers found that the predicted prevalence of the 3 elements of ACP differed by up 35% between patient characteristic subgroups, and was lower for 2 or more ACP elements among patients age 65 to 74 years, men, African Americans, Latinos, those with lower levels of educational attainment, and lower annual income. In addition, older adults with dementia had significantly lower predicted prevalence of having end-of-life discussions compared to patients without dementia (53.9% vs. 62.1%, p = 0.01). Patients with dementia were also less likely to have and advance care directives compared to patients without dementia (46.4% vs. 53.5%, p = 0.05). This study therefore shows that certain vulnerable patient populations may be less likely to engage in ACP. Targeted approaches should be explored as part of ensuring increased completion of ACP among members of these patient groups.
Surgical site infections (SSIs) remain the most common healthcare-associated infection. These infections contribute to increased length of hospital stay and often require readmission and/or ICU admission for wound-related complications. The role of hair removal at the surgical site in preventing SSIs remains unknown. Currently, the Centers for Disease Control (CDC) recommend that hair not be removed unless it is likely to interfere with surgery, in which case it should be removed immediately before surgery, preferably with electric clippers. In this randomized controlled trial, 1678 eligible patients were randomized to have removed from the surgical site with electric clippers or not, to study the role of hair removal in preventing SSI. Based on a per-protocol analysis, researchers found that the overall rate of SSI was 6.12% in the clipped group versus 6.32% in the non-clipped group (risk difference -0.20%, 95% CI -2.61% to 2.21%). When a modified intention-to-treat analysis was performed, the rate of SSI between groups also did not significantly differ, with 13.55% of patients in the clipped group having an SSI compared to 13.98% in the non-clipped group (risk difference -0.43%, 95% CI-3.73% to 2.86%). This study therefore shows that SSI rates do not significantly differ in patients that do or do not have hair clipped at the surgical site.
Image: PD
©2016 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.

![2 Minute Medicine: Pharma Roundup: Price Hikes, Breakthrough Approvals, Legal Showdowns, Biotech Expansion, and Europe’s Pricing Debate [May 12nd, 2025]](https://www.2minutemedicine.com/wp-content/uploads/2025/05/ChatGPT-Image-May-12-2025-at-10_22_23-AM-350x250.png)




