2 Minute Medicine Rewind September 11, 2017
Tiotropium in Early-Stage Chronic Obstructive Pulmonary Disease
Chronic obstructive pulmonary disease (COPD) has become increasingly prevalent with broad morbidity. In the early stages of COPD, defined as GOLD (Global Initiative for Chronic Obstructive Pulmonary Disease) stages 1 and 2, many patients exhibit very mild or no apparent respiratory symptoms. Tiotropium is a long-acting anticholinergic bronchodilator that improves airflow limitation in patients with moderate-to-severe COPD, reduces air trapping and exertional dyspnea. However, little is known regarding the treatment of COPD GOLD stage 1 and early stage 2 disease. In this randomized controlled trial, 388 patients age 40 to 85 years diagnosed with COPD GOLD stage 1 or 2 were randomized to receive either tiotropium 18 mcg once daily or matching placebo to investigate the effect of tiotropium on the FEV1 in these patients. The primary outcome was FEV1 at 1, 6, 12, 18, 24, and 25 months of follow-up. Researchers found that those who received tiotropium had a significantly greater FEV1 before bronchodilator use than those in the placebo group at 24 months (between-group difference 157 mL, 95% CI 123 mL to 192 mL, p<0.001). In addition, there was a significantly decreased rate of decline in FEV1 after bronchodilator use in the tiotropium group compared to the placebo group (difference 22 mL per year, 95% CI 6 mL to 3 mL 7 mL, p=0.006). There were also fewer COPD exacerbations in the intervention group compared to placebo (0.27 vs. 0.50 events per patient-year, RR 0.53, 95% CI 0.39 to 0.73, p<0.001). Limitations of this study included high withdrawal from care in both the tiotropium and placebo groups. Nonetheless, the use of tiotropium in early stages of COPD shows promise in improving FEV1 after bronchodilator use at 24 months compared to placebo, and helping to decrease COPD exacerbations.
Colorectal cancer (CRC) remains the second leading cause of cancer-related deaths in the United States. Screening programs can help decrease CRC incidence and mortality, but is limited by suboptimal adherence and underuse. In this randomized controlled trial, 5999 racially diverse patients age 50 to 64 years from disadvantaged socioeconomic backgrounds were randomized to receive either: 1) fecal immunochemistry test (FIT) outreach invitations for CRC screening by mail 2) colonoscopy outreach invitations for CRC screening by mail, or 3) usual care, where recommended in-person recommendations were made about CRC screening if indicated at clinic visits. The primary outcome was screening process completion within three years. Researchers found that screening process completion was achieved in 38.4% (95% CI 36.5% to 40.4%) of participants in the colonoscopy outreach group, 28.0% (95% CI 26.2% to 29.8%) in the FIT outreach group, and 10.7% (95% CI 9.1% to 12.6%) in the usual care group. Compared with the usual care group, screening process completion was 27.7% (95% CI 25.1% to 30.4%) greater in the colonoscopy outreach group and 17.3% (95% CI 14.8% to 19.8%) greater in the FIT outreach group. Compared to the greater in the FIT outreach group, screening completion was 10.4% (95% CI 7.8% to 13.1%) greater for the colonoscopy outreach group (p<0.001). Limitations of this study included the lack of in-depth decision tools, and failure to account for care provided outside this health system. This study was also not powered to capture differences in CRC detection and mortality. Nonetheless, the results of this study indicate that colonoscopy outreach may be effective in improving screening, although FIT also shows promise in improving screening when compared to usual care.
Hypertension is an important risk factor for events related to cardiovascular disease (CVD), end-stage renal disease (ESRD), and death from any cause. In this study, a secondary analysis of incident chronic kidney disease (CKD) and incident albuminuria was performed on a subgroup of patients that participated in SPRINT, a randomized controlled where participants without baseline CKD, had been randomized to either an intensive or standard systolic blood pressure (SBP) control group. Researchers found that at 6 months, there was a difference in adjusted mean estimated glomerular filtration rate (eGFR) of -3.32 mL/min/1.73 m2 (95% CI -3.90 to -2.74 mL/min/1.73 m2) between the intensive and standard SBP lowering groups. At 18 months, the difference was -4.50 mL/min/1.73 m2 (95% CI -5.16 to -3.85 mL/min/1.73 m2), with subsequent rates remaining relatively stable. At 3-years of follow-up, an incident CKD event occurred in 3.7% and 1.0% of participants of the intensive and standard groups, respectively (HR 3.54, 95% CI 2.50 to 5.02). Also at 3-year follow-up, the incidences of death or cardiovascular events were 4.9% and 7.1% of participants of the intensive and standard groups, respectively (HR 0.71, 95% CI 0.59 to 0.86). For each cardiovascular event or death from any cause prevented during the study, 1.2 incident CKD events were noted. This study therefore shows that while intensive SBP control results in significant decreases in cardiovascular and all-cause mortality, intensive SBP lowering is associated with an increased risk of incident CKD.
Reconciling the Effects of Screening on Prostate Cancer Mortality in the ERSPC and PLCO Trials
Conflicting results surrounding the value of prostate-specific antigen (PSA) screening has led the U.S. Preventive Services Task Force to state that screening has a very low impact in terms of preventing death from prostate cancer. In this retrospective study, researchers compared differences in implementation and practice settings to evaluate whether effects of screening on prostate cancer mortality relative to no screening differed between the European Randomized Study of Screening for Prostate Cancer (ERSPC) and Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial (PLCO), as well as estimate the effect of screening in both trials. The ERSPC had previously concluded that screening resulted a 21% reduction in prostate cancer mortality, while the PLCO screening trial found no difference in mortality between the control and intervention groups. With traditional analysis and extended analysis incorporating the mean lead time (MLT), which reflects the average time by which diagnosis is advanced by screening compared to the date of diagnosis without screening, researchers found no evidence that the effects of screening differed between trials ( p=0.37 to 0.47). However, there was strong evidence that the beneficial effects of screening increased with MLT (p=0.0027 to 0.0032). Specifically, the authors estimated that PSA screening reduces the risk of prostate cancer mortality by approximately 7%, resulting in a mortality rate of 9% per year of MLT. The ERSPC intervention group thus had an approximate risk reduction of 27% to 32% and the PLCO had an approximate risk reduction of 25% to 31% compared to the control groups. This study therefore shows that after accounting for differences in implementation and settings are accounted for, the results of ERSPC and PLCO provide evidence that PSA screening reduces prostate cancer mortality.
Racial and Ethnic Differences in Antibiotic Use for Viral Illness in Emergency Departments
Prior studies on pediatric emergency department (PED) use have shown race and/or ethnicity discrepancies in use, as well as various diagnostic and treatment strategies. However, no studies have examined the role of race and ethnicity in prescribing antibiotics in the PED. In this retrospective cohort study, researchers analyzed data from 39,445 patient visits (50.5% Non-Hispanic (NH) black, 46% female, 77.5% covered by Medicaid) from 7 academic PEDs to compare differences in antibiotic prescription rates for viral acute respiratory tract infections (ARTIs) based on race and ethnicity. Researchers found that antibiotics were prescribed at an average of 2.6% (95% CI 2.4% to 2.8%) of PED visits for viral respiratory illness. NH white children received antibiotics with the highest frequency (4.3%), followed by other NH children (2.9%), Hispanic children (2.6%), and NH black children (1.9%). NH white children were 2 times more likely to receive antibiotics than NH black children (OR 0.41, 95% CI 0.35 to 0.49) and roughly 1.5 times more likely than Hispanic children (OR 0.57, 95% CI 0.47 to 0.69). These differences persisted after adjusting for other demographics including age, provider type, and level of visit acuity. There was no significant difference found between provider type, with the majority of prescribers being pediatricians or PED attending staff. This study is consistent with other studies showing differences in care and management based on race and ethnicity. Overall, it suggests the need to further research factors contributing to these discrepancies, and shows that NH white children are more likely to be prescribed antibiotics for viral ARTIs in PEDs compared to children of color.
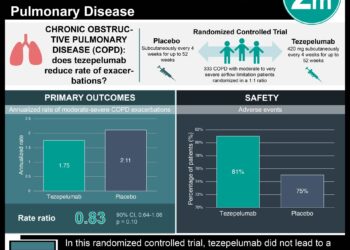
Image: PD
©2017 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.