2 Minute Medicine Rewind September 30, 2019
1. NIRS imaging in patients undergoing cardiac catheterization for suspected coronary artery disease can be used in identifying high-risk non-culprit lesions contributing to future major adverse coronary events.
Evidence Rating Level: 2 (Good)
Coronary artery disease is the leading cause of death worldwide. While modifiable risk factors are the target of reducing the risk of developing atherosclerosis, and therefore, coronary artery events, there are now increased efforts to identify vulnerable coronary plaques that are at an elevated risk of rupture. Near-infrared spectroscopy (NIRS) intravascular ultrasound imaging can be used to identify lipid-rich plaques (LRP). In this prospective cohort study, 1563 patients with suspected coronary artery disease undergoing cardiac catheterization with possible ad-hoc percutaneous coronary intervention (PCI) also underwent NIRS scanning of non-culprit segments to establish the relationship between LRPs detected by NIRS-intravascular ultrasound imaging at unstented sites and subsequent coronary events from new culprit lesions. As part of inclusion criteria in the study, patients must have had at least 50 mm of non-stented NIRS-intravascular ultrasound imaging data from at least two major coronary arteries. Of the patients that underwent NIRS intravascular ultrasound imaging, 1271 with analyzable maximum 4 mm lipid core burden index (maxLCBI) were followed up. The 2-year incidence of non-culprit major adverse coronary events (NC-MACE) was 9% (n=103). Researchers found that for each 100-unit increase in maxLCBI, patients had an increased risk of NC-MACE (HR 1.18, 95% CI 1.05 to 1.32, p=0.0043). This risk was further increased when assessing patients with a maxLCBI greater than 400 when compared to patients with a maxLCBI of 400 or less (HR 1.89, 95% CI 1.26 to 2.83, p=0.0021). This study therefore shows that NIRS imaging in patients undergoing cardiac catheterization for suspected coronary artery disease can be used in identifying high-risk non-culprit lesions. The findings of this study have important implications in reducing the risk of major adverse coronary events in a high-risk group.
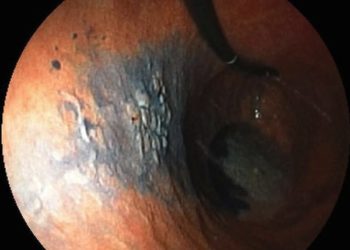
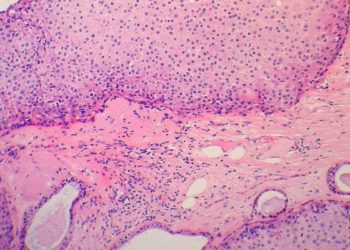
1. Patients undergoing laparoscopic distal gastrectomy for locally advanced gastric cancer have better postoperative outcomes when compared to those undergoing traditional ODG.
Evidence Rating Level: 1 (Excellent)
The use of multiple treatment modalities, including surgery, forms the current standard of care in the management of locally advanced gastric cancer. Over the last 20 years, the surgical approach to management has evolved from open gastrectomy to more minimally invasive techniques, including laparoscopic gastrectomy. While previous studies have shown that laparoscopy-assisted distal gastrectomy (LADG) is safe and offers faster postoperative recovery when compared to open distal gastrectomy (ODG), the safety and efficacy of this procedure in patients after the receipt of neoadjuvant chemotherapy has not been well studied. In this randomized clinical trial, 96 patients with locally advanced gastric cancer receiving neoadjuvant chemotherapy were randomized to undergo either LAD with D2 lymphadenectomy or ODG with D2 lymphadenectomy to evaluate the short-term outcomes of patients undergoing either procedure. Of note, in the per-protocol study population, the LADG group had significantly later ypN stage compared to the ODG group p=0.02). Nonetheless, researchers found that the LADG group had a significantly decreased postoperative complication rate (20% vs. 46%, p=0.007). Postoperative pain, as measured using a visual analog scale, was also lower in the LADG group (p=0.008), though significant findings were limited to postoperative day 2 only. Researchers also found that LADG patients demonstrated improved adjuvant chemotherapy completion (OR 4.39, 95% CI 1.63 to 11.80, p=0.003), with a decreased likelihood of terminating adjuvant chemotherapy due to adverse effects (p=0.04). This study therefore shows that patients undergoing LADG for locally advanced gastric cancer have better postoperative outcomes when compared to those undergoing traditional ODG. The decreased morbidity conferred through a laparoscopic approach may also improve tolerance to other treatment modalities such as adjuvant chemotherapy.
Treatment for nicotine use disorder among Medicaid-enrolled adolescents and young adults
1. The receipt of evidence-based treatment for nicotine use disorder is extremely low among adolescents and young adults.
Evidence Rating Level: 2 (Good)
It has now been well established that adolescents and young adults using e-cigarettes are at high risk of transitioning to combustible cigarettes. As such, it is important to determine the extent to which members of this young patient population with nicotine use disorder (NUD) receive evidence-based treatment with counseling and pharmacotherapy. In this retrospective cohort study, researchers used the Truven MarketScan Medicaid database to identify all individuals age 10 to 22 years with NUD and study the proportion of those receiving treatment within 6 months of NUD diagnosis. The receipt of treatment was confirmed using claims for counseling for NUD or pharmacy dispensing of nicotine replacement therapy, varenicline and sustained-release bupropion. Researchers found that among 81,144 youth identified with NUD with 6 months of follow-up after diagnosis, 3364 (4.1%) received counseling for NUD, 1095 (1.3%) received pharmacotherapy, and 110 (0.1%) received both counseling and pharmacotherapy. In assessing factors associated with the receipt of pharmacotherapy, researchers found that older age, white race, asthma (OR 1.26, 95% CI 1.02 to 1.56), depression (OR 1.36, 95% CI 1.02 to 1.81), anxiety disorder (OR 1.44, 95% CI 1.18 to 1.76), attention-deficit/hyperactivity disorder (OR 1.62, 95% CI 1.28 to 2.05), and co-occurring alcohol (OR 1.66, 95% CI 1.07 to 2.55) or marijuana use disorder (OR 1.36, 95% CI 1.02 to 1.81), increased the likelihood of receipt. Bupropion was the most commonly prescribed medication at 46.0%, followed by nicotine replacement therapy (31.2%) and varenicline (22.7%). A major limitation of this study is the fact that individuals not formally diagnosed with NUD would not have been included in this study; as such, the study population may not be reflective of the larger general population of adolescents and young adults with NUD. The sample also only included Medicaid enrollees, who are known to have higher rates of tobacco use than the general population. Patients formally diagnosed with NUD may also be more likely to seek out healthcare services, and therefore, the receipt of treatment for NUD may be inflated in this study population. Nonetheless, the findings of this study show that the receipt of evidence-based treatment for NUD among adolescents and young adults is extremely low. This has important implications for public health initiatives aimed at addressing NUD in this patient population.
1. Successful discontinuation of immune suppression after hematopoietic cell transplantation may be less likely in the setting of peripheral blood stem cell grafts.
Evidence Rating Level: 2 (Good)
Unlike solid organ transplantation, immune suppression discontinuation is commonly attempted after hematopoietic cell transplantation (HCT). The basis of this strategy lies in the thought that immune tolerance develops, that earlier immune suppression discontinuation supports graft vs. cancer effects, and decreases the risk of opportunistic infections. To date, however, little data is available on the rate of successful immune suppression discontinuation in this context. In this cohort study, 827 patients that had undergone allogeneic HCT were followed up to examine factors associated with successful immune suppression discontinuation and risk for immune suppression discontinuation failure. A total of 342 patients, 41.4% of the total study population, were able to stop immune suppression. However, 127 of these patients (37.1%) resumed immune suppression for treatment of graft-versus-host disease (GVHD). Factors associated with a decreased odds of immune suppression discontinuation included older receipt age (OR 0.27, 99% CI 0.14 to 0.50 for age >50 years vs. <30 years), mismatched unrelated donor (OR 0.37, 99% CI 0.14 to 0.97, p=0.008), peripheral blood graft vs. bone marrow graft (OR 0.46, 99% CI 0.26 to 0.82, p<0.001), and advanced stage of disease (OR 0.45, 99% CI 0.23 to 0.86, p=0.002). Failed attempts at immune suppression discontinuation resulting in GVHD was found to be associated with the use of peripheral blood stem cells (HR 2.62, 99% CI 1.30 to 5.29, p<0.001), prior GVHD, and earlier immune suppression discontinuation attempts. Of note, earlier discontinuation was not associated with decreased cancer relapse after transplantation (HR 1.95, 99% CI 0.88 to 4.31). This study therefore shows that successful discontinuation of immune suppression may be less likely in the setting of peripheral blood stem cell grafts, and that earlier attempts at discontinuation may not confer any long-term benefit with respect cancer relapse. This study has important implications in the identification of patients likely to succeed or not in discontinuation of immune suppression.
1. The risk of major cardiovascular events may be further reduced with the addition of fenofibrate therapy to statin treatment in adults with metabolic syndrome.
Evidence Rating Level: 2 (Good)
Metabolic syndrome is associated with an increased risk of atherosclerotic cardiovascular disease; this risk is partly attributable to accompanying atherogenic dyslipidemia. While statin therapy significantly reduces low density lipoprotein (LDL) cholesterol concentrations and therefore reduces the risk of cardiovascular disease, many patients continue to have significant cardiovascular risk. Fenofibrate has been suggested as a treatment option or adjunct in the management of dyslipidemia. Although previous large randomized clinical trials failed to demonstrate a reduction in major cardiovascular populations with diabetes, risk reduction was observed in subgroups with atherogenic dyslipidemia. In this population-based cohort study, adults in Korea age 40 years or older with metabolic syndrome receiving statin treatment (2007-2014) were followed up to evaluate the effects of fenofibrate treatment on major cardiovascular events (MACE) in adults with metabolic syndrome on statin therapy. Of the 29,771 individuals forming the initial cohort, 2156 participants were receiving combined treatment, and were thus weighted based on propensity scoring in a 1:5 ratio with 8549 patients using statin only treatment. Researchers found that the incidence per 1000 person-years of composite cardiovascular events was 17.7 (95% CI 14.4 to 21.8) in the combined treatment group, as compared to 22.0 (95% CI 20.1 to 24.1) in the statin-only group. This translated to a significantly reduced risk of cardiovascular events (HR 0.74, 95% CI 0.58 to 0.93). The risk of incident coronary heart disease, stroke, and cardiovascular death were also lower in the combined treatment group, however, these findings were not significant. This study therefore shows that the risk of major cardiovascular events may be further reduced with the addition of fenofibrate therapy to statin treatment in adults with metabolic syndrome.
Image: PD
©2019 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.