30% and 60% inspired oxygen fraction intraoperatively have similar prevalence of postoperative atelectasis
1. In postoperative patients randomized to receive either 30% FiO2 and 60% FiO2 via mechanical ventilation while under general anesthesia, there was no difference in the incidence of postoperive alectasis between the two groups.
Evidence Rating Level: 1 (Excellent)
A sizeable proportion of patients undergoing surgery with mechanical ventilation under general anesthesia develop postoperative atelectasis, which itself lends to longer hospital stays and increased 90-day mortality. The literature investigating which amount of inspired oxygen fraction (FiO2) is optimal for patients under general anesthesia has been conflicting. The current randomized controlled study investigated the effects of 30% versus 60% FiO2 without positive end-expiratory pressure (PEEP) and other recruitment maneuvers since most of the literature has either only compared very high FiO2 (80 to 100%) with low FiO2 (30 to 40%), or has made use of PEEP and recruitment maneuvers which may have interfered with the ability to infer causation about FiO2 use alone. A total of 120 patients undergoing neurosurgery were randomized into either the 60% or 30% FiO2 groups. They were also stratified by age (either < 60, or ≥ 60 years old). Patients would receive the same percentage of FiO2 after extubation and in the post-anesthesia care unit (PACU), and within half an hour of extubation, chest CTs were performed in order to measure postoperative atelectasis volume (as a % of total lung volume). A total of 113 patients (n = 55 in the 30% FiO2 group and n = 58 in the 60% FiO2 group) had their data analyzed. The overall incidence of postoperative atelectasis (representing > 1% of lung volume) in this study was 83.2%, but this was similar between both the 30% and 60% FiO2 groups. In addition to this, the percentage of postoperative atelectasis volume between the 30% and 60% FiO2 groups did not differ significantly (P = .121). There were also no significant differences between the groups with respect to over-aeration (P = .629), normal-aeration (P = .389), or poor-aeration volumes (P = .966). Overall, the results of this study suggest that a moderate FiO2 of 50-60%, which is more commonly used in the clinical environment, does not increase the risk for postoperative atelectasis. Future studies should elaborate on these results but also incorporate PEEP and recruitment maneuvers in order to understand best the implications of low and moderate FiO2 in a more realistic clinical environment.
Click to read the study in BMC Anesthestiology
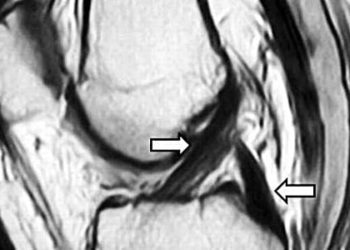
Image: PD
©2023 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.