Amyloid pathology may be detected decades prior to Alzheimer’s diagnosis
1. In this study, the presence of amyloid in patients without dementia was associated with age, APOE genotype, and presence of cognitive impairment.
2. In this study, when the prevalence of age-related and APOE genotype-specific amyloid positivity in individuals with normal cognition was compared to the age-related and APOE genotype-specific prevalence of Alzheimer’s disease type dementia, an association was detected with a time lag of about 20 to 30 years.
Evidence Rating Level: 2 (Good)
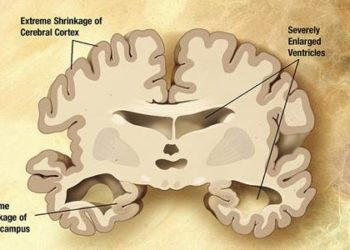
Study Rundown: Alzheimer’s disease, a debilitating and progressive mental illness, affects millions across the globe. A key marker to the diagnosis of Alzheimer’s disease (AD) is the presence of amyloid-β-aggregation in the brain. While the discovery of this pathology is often made well after the onset of symptoms, such a pathological change can be present 20 years prior to diagnosis. Prior studies have analyzed, with significant variability, the prevalence of such pathology in pre-demented patients.
This study evaluated the prevalence of amyloid-β-aggregate biomarkers in patients with normal cognition, subjective cognitive impairment (SCI), and mild cognitive impairment (MCI) and correlated it with known AD risk factors. This study found that the previously identified risk factors for AD of age and APOE genotype, were the same risk factors that were noted in this study to be associated with amyloid deposition in individuals with normal cognition, thus supporting the role of amyloid deposition as a marker of early AD. When the prevalence of age-related and APOE genotype-specific amyloid positivity in individuals with normal cognition was compared to the age-related and APOE genotype-specific prevalence of Alzheimer’s disease type dementia, an association was detected with a time lag of about 20 to 30 years. While strengths of this study include a participant-level analysis as well as a large number of studies evaluated, it may be weakened by a self-selection bias due to voluntary recruitment strategies. Based on these study results, it may soon be possible to identify early stage Alzheimer’s disease years before cognitive and behavioral symptoms emerge. Further research is required to evaluate risk assessment measures as well as the potential for anti-amyloid-β-therapies.
Click to read the study, published today in JAMA
Click to read the accompanying editorial, published today in JAMA
Relevant Reading: Toward defining the preclinical stages of Alzheimer’s disease: Recommendations from the National Institute on Aging and the Alzheimer’s Association workgroup
In-Depth [meta-analysis]: This meta-analysis included data from 2914 (38%) patients with normal cognition, 697 (9%) with SCI, and 3972 (52%) with MCI. Amyloid positivity was more common in patients with MCI compared with participants with normal cognition (mean difference 25%; 95%CI 22% to 28%; p < 0.001) or SCI (mean difference 23%; 95%CI 14% to 32%; p < 0.001). Across groups, amyloid deposition increased with age and APOE-ε4 carriers had a 10%-40% higher absolute prevalence than non-carriers. APOE genotype was associated with the age of onset of amyloid positivity, with the earliest amyloid deposition detected at 40 years for ε4ε4 carriers and the latest detected at 95 years for ε2ε3. Amyloid positivity when assessed in both an age-related and APOE genotype-specific manner and compared to AD risk in an age-related and APOE genotype-specific manner, respectively, revealed a time lag of about 20 to 30 years.
Image: CC/Wiki
©2015 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.