Computer-extracted MRI features help distinguish benign from malignant prostate lesions
1. In a retrospective review of prostate magnetic resonance imaging (MRI) and corresponding prostatectomy pathology specimens from 70 patients with prostate cancer, use of only the most discriminatory computer-extracted imaging features differentiating benign disease from cancer resulted in improved diagnostic capabilities.
2. Benign prostatic hyperplasia (BPH) was best discriminated from cancer using high-b-value diffusion-weighted imaging, while high grade cancer was best identified using the apparent diffusion coefficient.
Evidence Rating Level: 3 (Average)
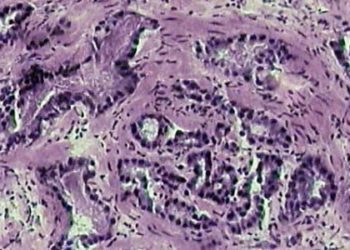
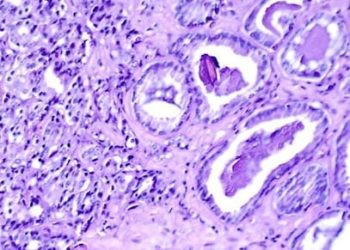
Study Rundown: Recent advancements in magnetic resonance imaging technologies, such as the development of multi-parametric MRI has demonstrated improved accuracy in the diagnosis and staging of prostate cancer. However, the use of image scoring systems such as the Prostate Imaging Reporting and Data System (PI-RADS) may lead to over-diagnosis of prostate cancer, particularly given the similar appearance of noncancerous mimics of prostate cancer such as prostatic intraepithelial neoplasia (PIN), BPH, prostatic atrophy, and prostate inflammation. The purpose of this study was to determine which computer-extracted features are best able to distinguish between benign and malignant prostate lesions. The authors retrospectively analyzed prostatectomy specimens from 70 men that underwent radical prostatectomy and had pre-operative multi-parametric MRI. The known areas of prostate cancer and non-malignant disease were co-registered to their corresponding images on multi-parametric MRI. Subvisual image features were algorithmically extracted to generate edge enhancement or highlight intensity homogeneity, among other textural features drawn from source images in an effort to focus attention on otherwise subtle differences in the appearance of different lesion types. Computer-extracted features were subsequently analyzed and associated with the respective pathological findings.
At the conclusion of the study, the authors found that each benign prostate disease-type analyzed (BPH, PIN, atrophy, and inflammation) had a distinguishing feature on multi-parametric MRI that may help to distinguish it from malignant prostatic adenocarcinoma. Key among these were the findings that BPH was best discriminated from cancer using high-b-value diffusion-weighted imaging, while inflammatory lesions were generally highly focal on contrast-enhanced images, and high-grade tumors were best differentiated using the apparent diffusion coefficient. The results of this study support the use of these computer extracted-MR to distinguish benign from malignant prostatic disease, and even found that using only the most useful differentiating feature to differentiate benign from malignant disease was more effective than using all available features. However, the study is limited by the small sample site and the lack of similar supporting data among other studies. Additional large trials are required to confirm these associations and more specifically delineate which features would be best used in daily practice, as would a trial that compares the use of these computer-extracted features to the diagnostic accuracy of simply reading of multi-parametric MRI images by an experienced radiologist.
Click to read the study in Radiology
In-Depth [retrospective cohort]: This study is a retrospective review of a cohort of 70 patients that underwent radical prostatectomy with pre-operative 3-T multi-parametric MRI. Sequences in the MRI included T2-weighted, diffusion-weighted, and dynamic contrast material-enhanced imaging. Each prostatectomy specimen was histologically investigated and digitized in consecutive sections. Each section was annotated for the presence of adenocarcinoma, BPH, PIN, atrophy, or inflammation by an experienced pathologist. The digitized slides were then co-registered with their corresponding area on the multi-parametric MRI images for direct comparison to known pathologic foci. At the conclusion of the study, each individual benign prostatic disease had a unique MR-derived feature that distinguished it from prostate cancer, which are as follows: BPH: lesions observed on high-b-value image; atrophy: focal lesion appearance on dynamic contrast-enhanced images; PIN: ADC values; inflammation: lesion focality on T2-weighted images. The accuracy of distinguishing specific benign lesions compared to cancer was improved when using only the single most useful differentiating factor computer-extracted feature (AUC = 0.70) versus grouping all noncancerous findings together compared to cancer (AUC = 0.62).
Image: PD
©2015 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.