Early repolarization on ECG not associated with long-term prognosis
1. From a retrospective cohort study, early repolarization (also known as J-wave, QRS slur or QRS notch) was not linked to increased risk of cardiovascular death at 10 years follow-up.
Evidence Rating Level: 2 (Good)
Study Rundown: Early repolarization (ER), defined as the J-wave pattern (also known as QRS slur or QRS notch), is an electrocardiogram (ECG) finding with a heterogeneous definition and an unclear association with long-term prognosis. It has been previously reported that, after about 7 years of follow-up, this wave pattern has no association with cardiovascular death. The goal of this retrospective cohort study was to determine this effect in veterans <56 years old using an initial resting 12-lead ECG. They were followed for a median of 17.5 years, with death by cardiovascular cause as the primary endpoint. The eligible patients were mostly white males and nearly 20% had ER in any lead, most often inferior leads. Comparison of patients with evidence of ER in inferior leads, lateral leads or both (with and without a downward ST slope) were not associated with an increased risk of cardiovascular death after 10 years of follow-up. The generalizability of this study may be limited because the cohort of veterans might not represent the general population. Nonetheless, this study suggests that ER may not be of prognostic value in predicting the long-term outcome of patients with these ECG wave patterns.
Click to read the study published today in the Annals of Internal Medicine
Relevant Reading: Role of Electrophysiological Studies in Predicting Risk of Ventricular Arrhythmia in Early Repolarization Syndrome
In-Depth [retrospective cohort]: This study looked at all ECGs of patients <56 years old at a single Veterans Affairs health center between 1987 and 1999. ECGs were manually coded for J waves defined as QRS notch (deflection ≥0.1mV at end of QRS) and QRS slur (abrupt slope change ≥0.1mV above baseline at the end of QRS) in 2 contiguous inferior (II, III, aVF) or lateral (V4-V6, I, aVL) leads. ECGs were excluded if they showed ER in anterior leads (associated with Brugada syndrome), were done in an ICU or were consistent with atrial fibrillation, pacemaker, accessory nodal pathway, bundle branch blocks or acute myocardial infarction. Eligible patients (20 661) were 57% white and composed mostly of men (90.5%) median age of 45 years and some women (9.5%) median age 41 years. Among all eligible patients there were 859 cardiovascular deaths (4.1%) and 157 (3.0%) among those with ER in any lead. However, at 10 years of follow-up the absolute risk difference for patients with ER in any lead (-0.57%, 95%CI −1.11 to −0.03%), inferior leads (-0.77%, 95%CI -1.27 to 0.27%), lateral leads (-1.07%, 95%CI -1.72 to 0.43%) or both (-1.36% 95%CI −2.06 to −0.65%) suggest that ER is not associated with the long-term prognosis of patients. The lack of association with prognosis persisted even if ER co-occurred with downward ST slope.
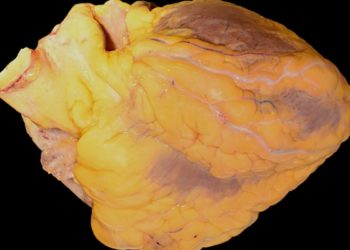
Image: PD
©2015 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.