Ultrasound enhances gastrointestinal absorption of drugs at low frequencies
1, Ultrasound can enhance the gastrointestinal delivery of drugs in porcine and rodent models through the cavitation of rectal tissue at low frequencies, increasing the permeability of the rectal and colonic tissues to multiple drugs, including macromolecules, without thermal or structural damage.
Evidence Rating: 2 (good)
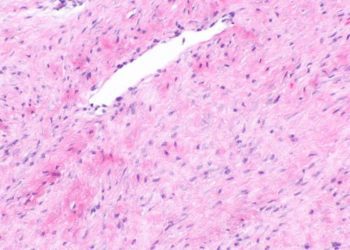
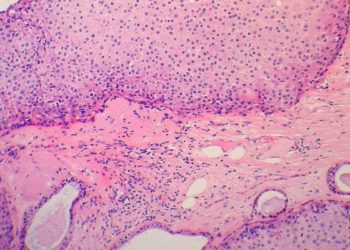
Study Rundown: Pathologies that affect the gastrointestinal (GI) mucosa often limit the efficacy of drugs delivered through the GI tract due to mucosal injury or rapid colonic transit, as in diarrheal states. In particular, macromolecular drugs such as monoclonal antibodies, peptides and nucleic acids are preferentially limited due to their bulky size. In this proof of concept study, low frequency ultrasound was used to increase the permeability of rectal tissue to enhance the delivery of drugs. Low frequency ultrasound causes a transient increase in permeability by using the sound pressure wave to physically propel therapeutic substances through tissue by a process known as transient cavitation. Various drugs, including glucose, insulin, hydrocortisone, and mesalamine were shown to have increased delivery when combined with low frequency ultrasound in an ex vivo model. Ultrasound also helped enhance drug delivery in an in-vivo swine model, effectively increasing drug delivery of both glucose and insulin. Rectal ultrasound was also shown to enhance drug delivery in a rodent model of colitis, increasing the absorption of mesalamine enemas, decreasing treatment times, and revealing superior histological scores for disease activity. This study proposes a novel utility for ultrasound in the therapeutic delivery of drugs through mucosal surfaces, particularly in disease states which benefit particularly from GI drug delivery, such as in inflammatory bowel disease. The study was limited in that it did not test the technique in outside of an animal model. Human trials would be necessary to validate the clinical efficacy of such a procedure, and to determine how feasible the rectal application of an ultrasound probe may be in practice. Additionally, concern is raised considering that such an application may be physically harmful in a patient with friable rectal tissue, such as in ulcerative colitis. Future studies examining the safety and efficacy of such an augmented form of drug delivery in humans is warranted, but also to determine if it would be an appropriate method to increase gastric, oral or subcutaneous drug absorption.
Click to read the study in Science Translational Medicine
Relevant reading: Oral drug delivery with polymeric nanoparticles: The gastrointestinal mucus barriers
In-Depth [animal study]: This study examined ultrasound-mediated drug delivery both in an ex-vivo model utilizing fresh gastrointestinal tissue and multiple in vivo trials in both mice and pigs. The ex-vivo component used GI tissue (colon and intestine) positioned between a donor chamber and a receiving chamber (a Franz diffusion cell) with a 20 and 40 kHz ultrasound probe, showing improved delivery of glucose (intestine: p < 0.003, colon: p < 0.002), insulin (intestine: p < 0.006, colon: p < 0.0005), hydrocortisone (intestine: p < 0.0003, colon: p < 0.0005), and mesalamine (intestine: p < 0.0006, colon: p < 0.00007). In an in-vivo porcine model, improved drug delivery was observed by a biologic feedback model, demonstrated by the delivery of insulin, a small peptide drug, the response to which was measured by the rate of fall of serum blood glucose both with and without ultrasound-mediated absorption assistance (P < 0.0004). Histological samples of the treated tissue did not show any significant epithelial or mucosal disruption, even over daily application of ultrasound over two weeks. In an in vivo rodent model of inflammatory colitis (dextran sodium sulfate-induced acute colitis), animals who were treated with 40-kHz ultrasound to aid the absorption of mesalamine enemas on a daily basis had faster resolution of colitis as compared to the same treatment every other day and to daily drug enemas without ultrasound (p < 0.00029). Tissue samples taken immediately after the application of ultrasound showed a 22-fold increase in local tissue concentration of mesalamine as compared to samples not treated with ultrasound, and NMR spectroscopy confirmed the chemical stability of the drug after ultrasound treatment.
Image: CC/Wiki/MorgueFile
©2015 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.




![[CORAL-1 trial] Interferon-free regimen for recurrent hepatitis C after liver transplant safe and effective](https://www.2minutemedicine.com/wp-content/uploads/2014/11/10229_lores-75x75.jpg)