Endovascular interventions appear superior to surgery in treatment of blister-like aneurysms
1. This systematic review and meta-analysis of patients with blister-like aneurysms examined neurologic outcomes and mortality differences between endovascular and surgical treatments, finding that endovascular repairs were associated with improved overall functional recovery and reduced mortality relative to surgical interventions.
2. Endovascular treatment was associated with more favorable neurologic outcomes in less severe cases (Hunt-Hess grade 3 or less) while surgical repairs were associated with more favorable outcomes in those with more severe presentations (Hunt-Hess grade 4 or greater.)
Evidence Rating Level: 1 (Excellent)
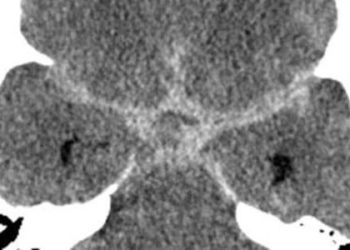
Study Rundown: Blister-like aneurysms are small, hemispherically-shaped lesions typically arising from the vasculature comprising the Circle of Willis, with lesions frequently found at nonbranching sites of the internal carotid artery (ICA). While pathogenesis of these aneurysms is uncertain, atherosclerotic weakening leading to vascular wall changes, hemodynamic stress and possible dissection have been suggested as possible causes. With an estimated incidence of 0.3%–1% of all intracranial aneurysms, these lesions are rare, yet they represent a potentially catastrophic cause of subarachnoid hemorrhage. Blister aneurysms are more likely to rapidly progress as compared to other aneurysms, with a high risk of rupture, intraoperative complications, and an increased likelihood of post-operative rebleeding. These characteristics impose technical challenges in both detection and treatment, and management of these fragile lesions must take into account their small size and atypical location. Therapeutic options for blister-like aneurysms include endovascular and surgical approaches; endovascular treatment involves balloon or stent-assisted coil placement within the aneurysm sac to stabilize the lesion, while deconstructive and reconstructive surgical approaches aim to isolate the lesion from the circulation.
The present study systematically reviewed and performed a meta-analysis of published literature that investigated whether endovascular management is associated with superior clinical and angiographic outcomes as compared to surgery, and sought to establish a treatment of choice. Symptoms at presentation, and post-treatment neurological and angiographic findings were compared between treatment techniques. The analysis determined that among patients with blister-like aneurysms, endovascular therapy was associated with a lower overall morbidity and mortality, and improved functional outcomes as compared to surgical approaches. However, after stratifying with respect to lesion severity on angiography, milder aneurysms, as graded by the Hunt-Hess scale, responded more favorably to endovascular therapy while those rated as severe were achieved superior outcomes following surgery. The authors highlighted the importance of radiographic evaluation and detection of blister-like lesion prior to treatment planning, and suggested additional studies in patients with suspected blister-like aneurysms to establish treatment recommendations. Although the conclusions of this study represent a significant step in evidence-based guidelines for the management of blister-like aneurysms, prospective studies are needed to better define the patient population in whom these methods will achieve favorable clinical outcomes.
Click to read the study in the American Journal of Neuroradiology
Relevant Reading: Blood blister-like aneurysms: single center experience and systematic literature review
In-Depth [meta-analysis]: A search of English-language articles published between January 1997 and November 2014 on “blood blister-like aneurysms” was performed and 60 studies in patients treated with surgery and endovascular methods were selected for this meta-analysis. The aggregated data included a total of 334 patients (246 females (73%) and 88 males with average age of 48.5 years). A total of 199 (59.5%) patients underwent endovascular intervention, while 114 (34.2%) patients received surgical treatment, and 19 patients (5.7%) received both treatments. The long-term neurological functional outcomes were assessed using a 7-point modified Rankin scale (mRS), in which a score of 0 to 2 was defined as “good”. Patient presentations were assessed using the Hunt-Hess (HH) and Fisher validated scales, which are clinical and radiographic scales of the severity of subarachnoid hemorrhages, and were found to be reliable outcome predictors in multivariable analysis in this study (HH, P = 0.041; Fisher P = 0.031). Endovascular treatment resulted in improved clinical outcomes overall, showing a favorable outcome (mRS 0-2) in 78.9% of patients as compared to 67.4% who underwent surgical intervention (P = 0.034). Among patients with lesions less than 1mm thick on CT scan (Fisher grade 2), a greater proportion (P = 0.081) of patients who underwent endovascular treatment (88.8%) achieved desirable outcomes (mRS 0-2) than patients receiving surgery (77.1%). Subgroup analysis was performed according to hemorrhage severity using the HH scale. With HH grade 4 or greater, the mortality rate among patients receiving endovascular therapy (37.0%) was significantly greater than the mortality rate in the surgery group (9.1%; P = 0.043). However, this pattern was reversed for HH grade 3 or lower, finding that mortality rates were significantly higher in the surgical subgroup (14.3%) as compared to the endovascular group (4.6%; P = 0.009). Angiographic findings of early occlusion status (complete, near-complete, and incomplete) were were 44.5%, 41.0%, and 14.5%, respectively, in patients receiving endovascular treatment and 76.9%, 18.1%, and 5.0% on follow-up (P = 0.001). Perioperative morbidity was identified in 7% of patients in this group (CI95: 3.0%–19.0%) with a mortality rate of 9% (CI95: 5.0%–13.0%). In patients who received surgery, early occlusion status on angiography was 96.4%, 3.6%, and 0.0%, respectively, and then 97.3%, 2.7%, and 0.0% (P= 0.001); 20.0% (CI95: 6.0%–49.0%) of patients in this group experienced preoperative morbidity, and preoperative deaths occurred in 10.7% (CI95: 5.0%–16.4%).
Image: PD
©2015 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.


![The ABCD2 score: Risk of stroke after Transient Ischemic Attack (TIA) [Classics Series]](https://www.2minutemedicine.com/wp-content/uploads/2013/05/web-cover-classics-with-logo-medicine-BW-small-jpg-350x250.jpg)