2 Minute Medicine Rewind March 12, 2018
Though there is limited evidence, opioids are often utilized in the management of chronic musculoskeletal pain. This randomized clinical trial, conducted over 12 months, aimed to compare opioids to non-opioid analgesics, with both interventions using treat-to-target strategies. Patients with moderate to severe chronic back pain or hip or knee osteoarthritis pain that had persisted despite analgesic use (n=240) were randomized to receive either opioid analgesics such as oxycodone, hydrocodone/acetaminophen and immediate-release morphine, or non-opioid analgesics including non-steroidal anti-inflammatory drugs (NSAIDs) and acetaminophen. The primary outcome was pain-related function, as measured using the Brief Pain Inventory (BPI) interference scale. Researchers found that there was no significant difference in pain-related function at 12 months of follow-up, with the opioid group having a mean BPI of 3.4 compared to the non-opioid arm with a mean BPI of 3.3 (difference 0.1, 95% CI -0.5 to 0.7). However, pain intensity was significantly lower in the non-opioid arm, as measured by the BPI severity scale, with a mean BPI that was 0.5 points lower (95% CI 0.0 to 1.0, p=0.03) compared to the opioid group. Finally, adverse effects were significantly more common in the opioid arm of the trial with a mean of 1.8 medication-related symptoms versus 0.9 symptoms in the non-opioid group (difference 0.9, 95% CI 0.3 to 1.5, p=0.03). Investigators therefore concluded that chronic opioid use is associated with more treatment-related adverse effects and does not improve pain-related function when compared to non-opioid medications.
Fluoroquinolone Use and Risk of Aortic Aneurysm and Dissection: Nationwide Cohort Study
Fluoroquinolone antibiotics may impact the extracellular matrix of vascular walls. Some observational studies have raised concerns surrounding the use of fluoroquinolones and the risk of aortic aneurysm or dissection. In this national retrospective cohort study, 360,088 Swedish patients treated with fluoroquinolones were matched via propensity score to patients treated with amoxicillin to investigate whether oral fluoroquinolone use is associated with an increased risk of aortic aneurysm or dissection, as measured by hospital admissions, emergency department visits, or deaths attributed to these diagnoses, within 60 days of treatment. Researchers found that the risk in the group treated with fluoroquniolones was 1.2 per 1000 person-years, as compared to a risk of 0.7 per 1000 person-years in the group treated with amoxicillin. Fluoroquinolone use was associated with a higher risk of aortic aneurysm or dissection (HR 1.66, 95% CI 1.12 to 2.46) and an absolute difference of 82 cases per 1 million treatment episodes (95% CI 15 to 181). Investigators therefore concluded that oral fluoroquinolones are associated with a higher risk of aortic aneurysm and dissection, as compared to amoxicillin.
Quadrupling Inhaled Glucocorticoid Dose to Abort Asthma Exacerbations
Acute asthma exacerbations are a major cause of morbidity and mortality amongst individuals affected by this chronic disease. In this randomized controlled, 1922 individuals were randomized to a self-management plan involving temporary quadrupling of inhaled glucocorticoid dose at the time of decline in asthma control, or the same plan without dose change for 12 months, in order to determine whether a temporary quadrupling could decrease the incidence of severe asthma exacerbations. Participating adults and adolescents with asthma had been receiving inhaled glucocorticoids, with or without other medications, and had had at least one exacerbation in the last year. Researchers found that a significantly lower proportion of patients in the quadrupling group experienced exacerbations, occurring in 45% of patients versus 52% of those in the non-quadrupling group (HR 0.81, 95% CI 0.71 to 0.92, p=0.002). However, the incidence of non-serious adverse events, including oral candidiasis and dysphonia, was significantly higher in the interventional arm of the study. Investigators therefore concluded that a self-management plan with temporary quadrupling of inhaled glucocorticoid dose with deterioration of asthma control resulted in fewer severe asthma exacerbations, as compared to no changes in dosing.
Control of blood pressure in patients with hypertension remains poor, despite the availability of effective treatments. Self-monitoring, as part of a self-management strategy, has been shown to improve blood pressure control. In this parallel, randomized controlled study, self-monitoring, with or without telemonitoring, was investigated for its efficacy when used in antihypertensive titration, as compared to usual care. Patients in the United Kingdom over the age of 35 with blood pressure greater than 140/90 mmHg were enrolled (n=1182) and were randomly assigned to either self-monitored blood pressure, self-monitored blood pressure with telemonitoring, or to usual care. Researchers found that after 1 year, systolic blood pressure was significantly lower in both self-monitoring groups, with a mean of 137 mm Hg in the group that only self-monitored and 136 mm Hg in the group that also used telemonitoring, as compared to usual care, which had a mean blood pressure of 140.4 mm Hg. The adjusted mean difference was -3.5 mm Hg for the self-monitoring group (95% CI -5.8 mm Hg to -1.2 mm Hg) and -4.7 mm Hg for the group that also telemonitored (95% CI -7.0 mm Hg to -2.4 mm Hg). No significant differences were found between the group that only self-monitored and the group that self-monitored and telemonitored. Investigators therefore concluded that self-monitoring, when used to titrate antihypertensive medications, results in significantly improved blood pressure control, whether or not telemonitoring is also used.
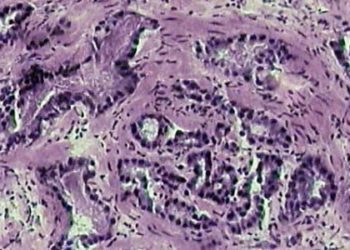
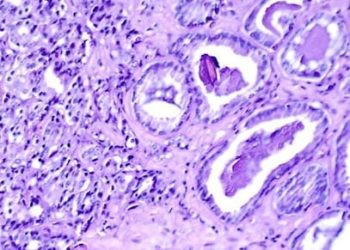
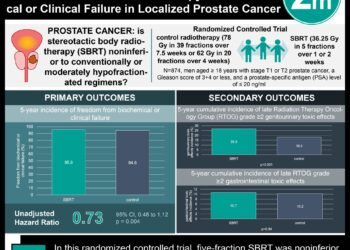
Prostate cancer screening utilizing prostate specific antigen (PSA) remains controversial, resulting in different recommendations worldwide. This randomized controlled trial aimed to evaluate the effect of a single PSA screening intervention with a standardized diagnostic pathway on mortality due to prostate cancer at a median follow-up of 10 years. Men age 50 to 69 years were enrolled (n=419,582) and randomized to receive an invitation to attend a PSA testing clinic and a single PSA test or receive standard practice without screening. In the group that received the invitation for screening, 40% attended the PSA clinic and 36% underwent PSA testing. Of these patients, 11% had a PSA value above 3 ng/mL and 85% of those patients underwent prostate biopsy. At a follow-up of 10 years, the mortality due to prostate cancer was not significantly different between the two groups, with 0.30 deaths due to prostate cancer per 100 person-years in the group that received invitations and 0.31 deaths per 1000 person-years in the standard practice group (rate difference -0.013 per 1000 person years, 95% CI -0.047 to 0.022; RR 0.96, 95% CI 0.85 to 1.08, p=0.50). All-cause mortality was also not significantly different between the two groups. However, the rate of prostate cancer diagnosis was higher in the intervention group (RR 1.19, 95% CI 1.14 to 1.25, p<0.001). Investigators therefore concluded that PSA testing for population-based screening does not result in a significant difference in prostate cancer mortality compared to standard practice without screening.
Image: PD
©2017 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.