2 Minute Medicine Rewind November 11, 2019
1. Bleeding after percutaneous coronary intervention (PCI) was more common in women, but the effect of two antiplatelet strategies on death and new Q-wave myocardial infarction following PCI did not differ between men and women.
Evidence Rating Level: 1 (Excellent)
Percutaneous coronary intervention (PCI) is a highly effective treatment in coronary artery disease. However, the optimal strategy of antiplatelet therapy after PCI remains debated. The randomized, controlled GLOBAL LEADERS study found that post-PCI, ticagrelor monotherapy (a P2Y12 inhibitor) following one month of dual antiplatelet therapy (DAPT) with aspirin was safe, but not superior to conventional DAPT in reducing the composite of all-cause mortality or new Q-wave myocardial infarction (MI). The objective of this pre-specified subgroup analysis of the GLOBAL LEADERS study was to compare two-year outcomes between all female and male participants, and the association between sex and the efficacy and safety of the two antiplatelet strategies. The primary endpoint was the composite of all-cause mortality and new Q-wave MI within two years after the index PCI. Of the 15,968 patients enrolled in the GLOBAL LEADERS study, 76.7% were men, and 23.3% were women. Analysis of baseline characteristics revealed that, compared with men, women were older, had a higher prevalence of diabetes, hypertension, and impaired renal function, were more likely to be nonsmokers, and had a lower prevalence of prior MI and previous treatment with PCI and coronary artery bypass graft surgery. Researchers found that there was no difference in the primary endpoint between men and women (3.90% vs. 4.75% respectively, adjusted HR 1.00, 95% CI 0.83 to 1.20). However, women had a higher risk of Bleeding Academic Research Consortium type 3 or 5 bleeding (adjusted HR 1.32, 95% CI 1.04 to 1.67) and hemorrhagic stroke (adjusted HR 4.76, 95% CI 1.92 to 11.81) at two years. There was no between-sex difference in the efficacy and safety of the two antiplatelet strategies at two years, but at one year, ticagrelor monotherapy was associated with a lower risk of bleeding in men (HR 0.72, 95% CI 0.53 to 0.98) but not in women (HR 1.23, 95% CI 0.80 to 1.89, p for interaction = 0.045). In summary, this study suggests that women are at a higher risk of bleeding and hemorrhagic stroke after PCI, and that ticagrelor monotherapy may be associated with a decreased risk of bleeding at one year after PCI in men, but not in women.
1. Lung injury associated with e-cigarettes or vaping is a new disease entity that can be treated effectively with steroids; however, residual lung abnormalities often persist.
Evidence Rating Level: 1 (Excellent)
There is currently an outbreak of lung injury associated with e-cigarettes or vaping (E-VALI or VALI) in the USA. The objective of this prospective observational cohort study was to describe the clinical course, treatment, and short-term outcomes of E-VALI. Data was collected on 60 patients with E-VALI secondary to vaping exposure to nicotine, tetrahydrocannabinol, or both, from different hospitals throughout the state of Utah. A case series definition of pulmonary infiltrates (on chest radiograph or chest CT, or both) in a patient with a history of e-cigarette use or vaping in the 90 days before symptom onset, and exclusion of an alternative diagnosis, was used. Overall, frequency of vaping varied from one or two times per week to over 50 times per day. 23% of patients had a history of asthma, and 32% had a history of depression or anxiety, but otherwise, patients did not lung injuhave significant comorbidities. 88% of patients presented with constitutional symptoms, 98% with respiratory symptoms, and 90% with gastrointestinal symptoms. Tachycardia (83%), elevated white blood cell count (>11,000 per mm3) (77%), and tachypnea (72%) were the most common clinical signs. Notably, when measured, inflammatory markers were often severely high, with a median C-reactive protein concentration of 31 mg/L (IQR 21 to 33), and a median erythrocyte sedimentation rate of 92 mm/h (IQR 65 to 103). 55% of patients were admitted to the intensive care unit (ICU). Patients were treated primarily with antibiotics (90%), steroids (95%), and supplemental oxygen (88%). The main therapy that treating clinicians believed led to rapid improvement within days was steroids. Ten percent of patients were readmitted to an ICU or hospital within 2 weeks, half of whom had relapsed with vaping or e-cigarette use. Of 26 patients who were followed up within 2 weeks, despite clinical and radiographic improvement in all, 67% (10 of 15) had residual abnormalities on chest radiographs, and 67% (6 of 9) had residual abnormalities on pulmonary function testing. Two patients died, and lung injury associated with e-cigarettes or vaping was thought to be a contributing factor, but not the primary cause of death, for both. In summary, this study suggests that E-VALI is associated with respiratory, gastrointestinal and constitutional symptoms, and is often associated with residual radiographic and spirometric abnormalities despite short-term improvements with treatment.
1. Utilizing geriatric assessment in oncology clinical visits for older adults with advanced cancer improves patient-centered communication about aging-related concerns.
Evidence Rating Level: 1 (Excellent)
Patient-centered communication is of critical importance in oncologic care. Previous studies have demonstrated the benefits of interventions that facilitate oncologist-patient communication, but these interventions were not tailored to address aging-related concerns of older patients, despite the fact that older adults generally represent the majority of patients with advanced cancer. Geriatric assessment (GA) uses validated patient-reported and objective measures to capture domains important to older adults; to date, no studies have evaluated the impact of GA on oncology patient satisfaction. The objective of this cluster-randomized, controlled trial was to examine whether the provision of a GA summary and GA-guided recommendations to oncologists can improve communication about aging-related concerns. Five hundred and forty one participants with 414 caregivers across 31 oncology practices were enrolled, and assigned to receive either a tailored GA summary with recommendations for each enrolled patient (intervention), or alerts only for patients meeting criteria for depression or cognitive impairment (usual care) to study the impact on patient satisfaction with communication about aging-related concerns (modified Health Care Climate Questionnaire; score range 0-28, higher scores indicate greater satisfaction). Researchers found that patients in the intervention group were more satisfied with communication about aging-related concerns that those in the usual care group (difference in mean score 1.09 points, 95% CI 0.05 to 2.13 points, p=0.04). Satisfaction remained higher in the intervention group over 6 months (difference in mean score 1.10, 95% CI 0.04 to 2.16, p=0.04). There were significantly more aging-related conversations in the intervention group’s visits (difference 3.59, 95% CI 2.22 to 4.95, p<0.001). Caregivers in the intervention group were more satisfied with communication after the visit (difference 1.05, 95% CI 0.12 to 1.98, p=0.03). However, quality of life outcomes did not differ between groups. Overall, this study supports the integration of a geriatric assessment into community oncology care in terms of patient and caregiver-reported outcomes.
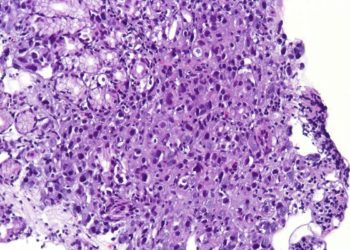
Polatuzumab Vedotin in Relapsed or Refractory Diffuse Large B-Cell Lymphoma
1. Polatuzumab vedotin in combination with bendamustine and rituximab yielded higher complete response rates than bendamustine and rituximab alone.
Evidence Rating Level: 1 (Excellent)
Diffuse large B-cell lymphoma (DLBCL) is often curable, but a portion of patients are refractory to, or relapse after, treatment with the current standard of care (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone chemoimmunotherapy). Some of these relapsed/refractory (R/R) patients are cured with autologous stem-cell transplantation (ASCT), but few options exist for patients who are ineligible for ASCT. Polatuzumab vedotin, a CD79b-targeted antibody conjugate delivering monomethyl auristatin E, a microtubule inhibitor, has demonstrated encouraging activity in this setting, thus there is impetus to combine it with CD20-targeted agents such as obinutuzumab and rituximab. These combinations were tested in the present phase Ib/II study. In the phase Ib study, the safety and efficacy of polatuzumab vedotin with bendamustine and obinutuzumab (pola-BG) and polatuzumab vedotin with bendamustine and rituximab (pola-BR) was evaluated in 6 and 6 patients with R/R DLBCL who are inelibible for ASCT, respectively. In the randomized, controlled phase II portion, an expansion cohort evaluating pola-BG (21 patients) and a randomly assigned cohort (80 patients; 40 per treatment arm) comparing pola-BR with BR alone, were studied to determine the complete response (CR) rate of pola-BR versus BR as measured by PET-CT. Researchers found that the phase Ib/II pola-BG cohort (n = 27) had a CR rate of 29.6% and a median OS of 10.8 months (median follow-up, 27.0 months). In the randomized cohort (pola-BR and BR groups), pola-BR patients had a significantly higher CR rate (40.0% vs. 17.5%, p=0.026) and longer progression-free survival (median 9.5 vs. 3.7 months, HR 0.36, 95% CI 0.21 to 0.63, p=0.001) and overall survival (median 12.4 vs. 4.7 months, HR 0.42, 95% CI 0.24 to 0.75, p=0.002; median follow-up, 22.3 months) than BR patients. Overall, the small number of patients in the pola-BG cohort made estimation of the true CR rate difficult, but there was no indication of benefit of obinutuzumab over rituximab in this setting. Pola-BR patients had higher rates of grade 3-4 neutropenia (46.2% vs. 33.3%), anemia (28.2% vs. 17.9%), and thrombocytopenia (41% vs. 23.1%), but similar grade 3-4 infections (23.1% vs. 20.5%), as compared with the BR group. Pola-BG had a tolerable safety profile. In summary, this study supports a role for polatuzumab vedotin in combination with BR, but larger studies are required to validate the clinical efficacy of this therapeutic approach.
1. The glucocorticoid-induced TNF receptor-related protein agonist, BMS-986156, is safe and tolerable as monotherapy and in combination with nivolumab.
Evidence Rating Level: 2 (Good)
Although immune checkpoint inhibitors (ICI) have shown clinical efficacy in a wide variety of cancers, a significant portion remain unresponsive to checkpoint blockade. Therefore, new strategies for modulating the critical balance of T-cell activation and antigen tolerance are needed. Agonistic antibodies targeting the glucocorticoid-induced TNF receptor-related protein (GITR) have been hypothesized to synergize with and augment the effect of ICIs. The GITR-agonist BMS-986156 was engineered to increase T-cell activation and deplete intratumoral regulatory T cells. In this open-label, non-randomized, phase I/IIa study, 292 patients with advanced solid tumors and an Eastern Cooperative Oncology Group (ECOG) performance status of 1 or less were assigned to either BMS-986156 as monotherapy at varying doses (10, 30, 100, 240, or 800 mg), or in combination with 240mg of nivolumab every 2 weeks. One cohort also received 480 mg of BMS-986156 plus 480 mg of nivolumab every 4 weeks. The primary endpoints were safety, tolerability, and dose-limiting toxic effects. Key secondary endpoints included antitumor activity and exploratory biomarker analyses. The monotherapy cohort included 34 patients (4 patients completed initial treatment), and the BMS-986156 cohort included 258 patients (65 patients completed initial treatment). Baseline characteristics were similar between the monotherapy and combination therapy cohorts. Researchers found that the safety profile of BMS-986156 was tolerable; no grade 3 to 5 treatment-related adverse events occurred with BMS-986156 monotherapy; grade 3 to 4 treatment-related adverse events occurred in 24 patients (9.3%) receiving BMS-986156 plus nivolumab, with no grade 5 treatment-related adverse events. There was a trend towards an increase in CD8+ T-cell and natural killer cell proliferation after administration of both BMS-986156 monotherapy and combination therapy, although these results were not statistically significant. No clinical responses were seen with BMS-986156 monotherapy, and objective response rates ranged from 0% to 11.1% across combination therapy cohorts, similar to historically observed objective response rates with anti-PD-1 therapy alone. This study was limited by the lack of comparator groups, such as a nivolumab monotherapy group; therefore, the contribution of the GITR agonist to the clinical activity of the combination therapy remains unclear. Overall, this study highlights the safety and tolerability of the GITR agonistic antibody BMS-986156 with or without nivolumab, but further studies with comparator groups are warranted to determine if this therapy is an effective strategy in a broad patient population.
Image: PD
©2019 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.