2 Minute Medicine Rewind February 22, 2021
1. Among patients with incident atrial fibrillation, the use of non-vitamin K antagonist oral anticoagulants compared with warfarin was associated with a decreased risk of dementia.
Evidence Rating Level: 2 (Good)
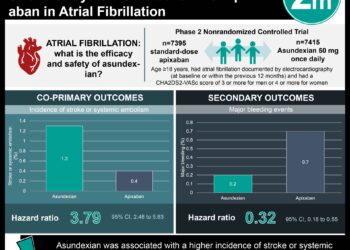
While the incidence of both atrial fibrillation (AF) and dementia continue to rise in an aging world, it has been well documented that AF is associated with a higher risk of developing dementia. Mainstays of treatment for AF include warfarin and non-vitamin K antagonist oral anticoagulants (NOAC), like apixaban and rivaroxaban, and plausibly may delay the development of AF-related microbleeds with ensuing dementia. As such, this nationwide cohort examined whether the risk of dementia among patients with AF differs between users of warfarin and NOACs. The primary outcome was the incidence of dementia. In particular, the risk of dementia between warfarin and NOAC users was investigated. 25,089 patients with incident AF were recruited and, after propensity matching, the NOAC (mean [SD] age = 70.3 [11.7] years, 59.5% male) and warfarin (mean [SD] age = 70.4 [11.6] years, 59.0% male) cohorts each included 6,034 patients. Dementia was diagnosed in significantly fewer patients in the NOAC cohort than in the warfarin cohort (304 vs. 360, p = 0.0285). Furthermore, in a stratified analysis, the risk of dementia was lower among patients using NOACs when compared with warfarin if aged 65 to 74 years, if at a high risk of stroke as measured by the CHA2DS2-VASc score, and if at a high risk of bleeding as measured by the HAS-BLED score. A final analysis with the removal of propensity score matching showed that the NOAC cohort had a persistently lower risk of dementia compared with the warfarin cohort (aHR 0.86, 95% CI 0.77 to 0.97, p = 0.0106). In all, this large, nationwide cohort study is among the first to report that among those with incident AF, the use of NOACs is associated with a decreased risk of dementia, particularly among those aged 65 to 74 years and having a higher risk of stroke or bleeding. It is noteworthy however, that the study failed to include potential confounding variables in its analysis including lifestyle and environmental factors, and may also introduced selection bias in its study design. Future studies in the form of randomized controlled trials are encouraged to provide further insight into the topic.
Higher SARS-CoV-2 infection rate in pregnant patients
1. In Washington State, pregnant patients were found to be at a higher risk of SARS-CoV-2 infection.
2. Results were more pronounced if patients belonged to a non-white racial or ethnic group or received their care in a language other than English.
Evidence Level Rating: 2 (Good)
As the COVID-19 pandemic continues to exert a broad impact on global health systems, an understanding of groups at higher risk is important not only for triage but also public health interventions. In that vein, this retrospective cohort study from Washington State sought to estimate and compare the infection rates in pregnant patients with similarly aged adults, as well as examine disparities by race/ethnicity and language use. Patients across 35 hospitals and clinic systems were included for analysis. 240 cases of SARS-CoV-2 infections in pregnant patients were detected, 15.8% in the first trimester, 27.9% in the second, and 56.3% in the third. The overall infection rate in pregnancy among trial sites was 13.9/1,000 deliveries. When comparing this to the overall infection rate among those aged 20-39 years in Washington State (7.3/1,000), the infection rate in pregnancy was a significant 1.7 times higher. Furthermore, when compared with those who delivered live births in Washington State in 2018, the proportion of infections in pregnancy among most racial and ethnic minority groups was 2.0 to 3.9-fold higher. In contrast, the proportion of white and Asian pregnant women with infection was lower than expected based on 2018 data. Finally, a disproportionate number of pregnant patients experienced SARS-CoV-2 infections if receiving their care in a non-English language. Though a selection bias may have been introduced due to the incomplete collection of all cases in the state, this retrospective cohort study revealed that the SARS-CoV-2 infection rate is higher among pregnant patients compared with similarly aged non-pregnant patients, and that nearly all non-white racial and ethnic groups are disproportionately affected. Having a robust understand of the patterns of infection can help unravel the social structures impacting the spread of disease and contribute to the design of effective and equitable public health interventions.
1. Among patients with and without COPD, a greater magnitude of pulmonary arterial pruning as measured by CT imaging was associated with a faster progression of percent emphysema as well as a faster decline in FEV1/FVC.
Evidence Level Rating: 2 (Good)
Chronic obstructive pulmonary disease (COPD), including emphysema, is a leading cause of morbidity and mortality worldwide. Additionally, a greater “percent emphysema,” or the percentage of emphysema-like lung measured on CT scan, is associated with greater lung function decline as well as mortality. It is unknown, however, if differences in pulmonary parenchymal vasculature contribute to the progression of emphysema and COPD. Therefore, this study sought to evaluate whether pulmonary artery “pruning” – as measured by the decrease in the ratio of small artery volume to the total pulmonary artery volume on CT imaging – is associated with a more rapid progression of percent emphysema and thus decline in lung function. 4,227 ever-smoking participants (mean [SD] age = 60 [9] years, 50% female) were included for analysis, 47% of whom were current smokers and 41% of whom had a diagnosis of COPD. Among study participants, median percent emphysema was 2.1% (IQR 0.6% to 6.3%). After adjusting for baseline percent emphysema and FEV1, it was found that greater pulmonary artery pruning was associated with a more rapid progression of percent emphysema (0.11% per year per SD arterial pruning, 95% CI 0.09 to 0.16) as measured by CT imaging. Pulmonary venous pruning also predicted a faster rate of percent emphysema progression, though to a lesser magnitude. Furthermore, arterial pruning was found to be associated with a faster decline in FEV1/FVC ratio (-0.04% per year per SD arterial pruning, 95% CI -0.008 to -0.001, p = 0.042), a spirometric classification used to determine the severity of airflow limitation. In all, this study suggests that greater pulmonary arterial pruning as seen on CT imaging is associated with a more rapid decline in lung function among patients with and without COPD, adding to prior data showing the importance of pulmonary vasculature in the pathogenesis and progression of emphysema and COPD.
The benefits and harms of antibiotic prophylaxis for urinary tract infection in older adults
1. Among older adults with urinary tract infections, antibiotic prophylaxis was associated with an increased risk of ED visit or hospitalization for UTI, sepsis, or bacteremia.
Evidence Level Rating: 2 (Good)
Urinary tract infections (UTI) are the most common bacterial infections prompting the utilization of health care services. They exert a significant burden on patients and providers, particularly for older adults, with the threat of bacteremia and sepsis. Some patients with recurrent UTIs are managed with prophylactic antibiotics to reduce the incidence of repeat infection; however, the evidence for this strategy with regards to more severe outcome measures, particularly among older adults, is unknown. This retrospective cohort study compared older adults ≥ 66 years receiving antibiotic prophylaxis for UTI – defined as duration ≥ 30 days following a positive urine culture – to matched patients with a positive urine culture who did not receive prophylaxis. The primary efficacy outcome was a composite of ED visits or hospitalization for UTI, sepsis, or bacteremia within 30 days to one year after the positive urine culture. The primary harm outcome was detection of a repeat urinary isolate resistant to an antibacterial agent to which it was initially susceptible. Matching yielded 3,190 UTI prophylaxis patients and 30,542 control patients. It was found that 4.7% of the prophylaxis cohort and 3.6% of the control cohort required ED visits or hospitalization for UTI, sepsis, or bacteremia (HR 1.33, 95% CI 1.12 to 1.57); this increased utilization was particularly pronounced among patients less than 80 years of age (HR 1.66, 95% CI 1.33 to 2.06). Furthermore, the acquisition of antibiotic resistance to any agent was more pronounced in the prophylaxis cohort (HR 1.31, 95% CI 1.18 to 1.44). Finally, antibiotic-associated harm was more common among patients in the prophylaxis cohort, with the risk of C. difficile infection and medication adverse side effects being significantly higher. In all, among older adults with a history of positive urine culture, antibiotic prophylaxis was associated with an increased risk of harm as well as an increased risk of ED visit or hospitalization for UTI, sepsis, or bacteremia, suggesting that the harms of UTI prophylaxis in this cohort may outweigh the benefits.
1. Early head-to-pelvis CT imaging for patients experiencing out-of-hospital circulatory arrest is safe, expedites diagnosis, and can meaningfully impact management.
Evidence Level Rating: 2 (Good)
Out-of-hospital circulatory arrest (OHCA) is a devastating event. For patients resuscitated from an OHCA event, determining the etiology is often challenging due to a lack of medical history and communication barriers posed by potential altered mentation and/or the need for intubation. As such, this prospective cohort study was designed to evaluate the early use (≤ 6 hours from hospital arrival) of head-to-pelvis CT imaging in patients resuscitated from an OHCA event. The imaging protocol used in this study included a non-contrast head CT from the top of the head to below the mandible, an ECG-gated CT scan of the thorax, and a non-ECG gated venous phase CT scan extending from the diaphragm to just below the pelvis. Images were reviewed by radiologists blinded to patient clinical data. The primary study outcomes were the number of OHCA causes identified by the imaging protocol and the frequency with which the imaging protocol identified critical findings that did or should affect management. 104 patients were ultimately included for analysis, with a mean time to imaging from hospital arrival of 1.8±0.8 hours. The imaging protocol identified 39% of the adjudicated causes for OHCA and 95% of causes potentially identifiable on CT. Of the 44 patients with time-sensitive diagnoses that required change in management, the imaging protocol identified 98%. In 13% of cases, the cause of OHCA was determined exclusively by CT imaging, and would not have otherwise been detected. Of note, no inappropriate treatments were performed based on CT imaging findings and there were no allergic reactions to contrast dye. Overall, this prospective study demonstrated that a head-to-pelvis CT imaging protocol in the setting of OHCA had high diagnostic utility to identify and rule out causes of circulatory arrest. These data suggest that early head-to-pelvis CT imaging for patients with OHCA is safe, expedites diagnosis, and can meaningfully impact management.
Image: PD
©2020 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.