Clopidogrel monotherapy is superior to aspirin monotherapy for chronic maintenance after percutaneous coronary intervention
1. Clopidogrel monotherapy reduced long-term rates of all-cause mortality, non-fatal myocardial infarction, and stroke after drug-eluting stent placement compared with aspirin monotherapy.
2. The superiority of clopidogrel was seen for both thrombotic and bleeding endpoints and was consistent across demographic groups.
Evidence Rating Level: 1 (Excellent)
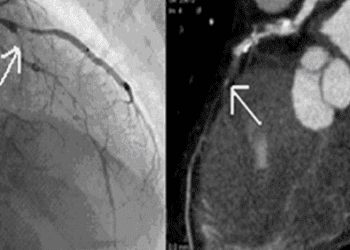
Study Rundown: Patients who receive percutaneous coronary intervention (PCI) with a drug-eluting stent (DES) are recommended to start dual anti-platelet therapy (DAPT) for 6-12 months after intervention and transition to indefinite monotherapy for chronic management. Current guidelines recommend aspirin as the first line option for chronic monotherapy; clopidogrel, a P2Y12 inhibitor, is recommended for those who cannot tolerate aspirin. This prospective, randomized, open-label, multicenter clinical trial (HOST-EXAM) compared the efficacy of clopidogrel monotherapy and aspirin monotherapy for chronic maintenance after PCI with DES. The results of this study demonstrate lower rates of all-cause mortality, as well as thrombotic and bleeding events during the 24-month follow-up period in patients who received clopidogrel monotherapy compared with those who received aspirin monotherapy. These results support the use of clopidogrel for chronic management after PCI to prevent adverse clinical events.
Click to read the study in the Lancet
Relevant Reading: Effects of pretreatment with clopidogrel and aspirin followed by long-term therapy in patients undergoing percutaneous coronary intervention: the PCI-CURE study
In-Depth [randomized controlled trial]: This study included 5438 patients who had maintained DAPT following PCI with DES from 37 centers in South Korea. Participants were randomly allocated to clopidogrel (n=2710) and aspirin (n=2728) monotherapy groups in a 1:1 ratio. Patient demographics and baseline characteristics were comparable among groups. Primary endpoint was defined as a composite measure of all-cause death, non-fatal myocardial infarction, stroke, readmission due to acute coronary syndrome, and major bleeding events within the 24-month follow-up window. Secondary endpoints included revascularization procedures, stent thrombosis, and major gastrointestinal complications.
In the follow-up period, 5.7% of patients in the clopidogrel monotherapy event had a primary endpoint event versus 7.7% in the aspirin monotherapy group (hazard ratio [HR] 0.73 [95% CI 0.59-0.90]; p=0.0035). Event rates in all subcomponents of the primary composite endpoint favored clopidogrel monotherapy. Based on Kaplan-Meier curves, differences in event rates emerged approximately 9 months after respective clopidogrel or aspirin monotherapy initiation. The results of this study are limited by potential underreporting of events after study initiation, as event rates were lower than expected, and limited the follow-up time. However, the results of this study support the launch of the 10-year extended HOST-EXAM trial, the results of which could change the current clinical recommendation for chronic maintenance therapy after PCI with DES.
Image: PD
©2021 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.