Tranexamic acid is unlikely to induce signs suggestive of cerebral ischemia in the treatment of acute intracerebral hemorrhage: TICH-2 study
1. Patients presenting with acute intracerebral hemorrhage were not more likely to have diffuse-weighted imaging hyperintense lesions (DWIHL), suggestive of cerebral ischemia, on magnetic resonance imaging following administration of tranexamic acid.
2. Patients who received tranexamic acid (TXA) within 3 hours of intracerebral hemorrhage onset were less likely than controls to have DWIHL on imaging.
Level of Evidence: 1 (Excellent)
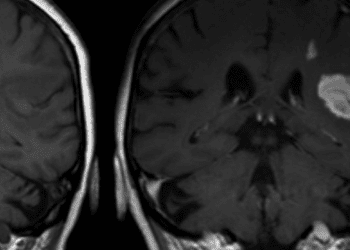
Study Rundown: The presence of spatially-distinct diffusion-weighted imaging hyperintense lesions (DWIHL) occurs in up to 40% of patients presenting with acute intracerebral hemorrhage (ICH), particularly in those whose ICH is attributable to hypertensive arteriopathy. The etiology of DWIHLs in the context of ICH is not definitively known although local ischemia is thought to play a role. Tranexamic acid (TXA) is a hemostatic agent used for a number of indications, including ICH. However, other studies have hypothesized that prothrombotic agents such as TXA may contribute to cerebral ischemia and could be implicated in the pathogenesis of DWIHL seen on magnetic resonance imaging (MRI). The present study sought to evaluate this theoretical relationship. This was a substudy of a randomized clinical trial of 219 patients (TICH-2 trial). 96 (44%) of patients underwent TXA therapy while the remaining 56% were controls. The prevalence of DWIHLs amongst all study participants was 21.9% (48), most commonly detected within the cerebral lobes. There was no significant difference in the number of DWIHLs detected amongst the TXA group and the control group. Subgroup analysis identified that patients with significant cerebral amyloid angiopathy were more likely to have DWIH, and that patients with a history of chronic infarct were less likely to develop new lesions following TXA therapy. Finally, patients who had DWIHL detected within two weeks of the index event were more likely to have an ischemic stroke within 90 days compared to those who had clear brain imaging. This randomized controlled trial identified no clear increase in risk of DWIHL following management of ICH with TXA therapy, other than in a select subgroup of patients. Some strengths of this study include the randomized, multicentre trial design which does well to control for confounding variables. A drawback is the relatively small sample size due to stringent selection criteria which reduces the generalizability of the study’s findings. Future research should focus on confirming these findings in a larger population.
Click to read the study in JAMA Neurology
Click to read an accompanying editorial in JAMA Neurology
Relevant reading: Acute ischaemic brain lesions in intracerebral haemorrhage: multicentre cross-sectional magnetic resonance imaging study
In-depth [randomized controlled study]: This was a substudy reporting the results of the Tranexamic Acid for Hyperacute Pulmonary Hemorrhage (TICH-2) trial, a multicentre, randomized controlled trial. Patients were recruited between March 1, 2013 and September 30, 2017 from over one hundred countries. Participants were randomized in a 1:1 fashion to receive either tranexamic acid or placebo within 8 hours of onset of ICH. The dosage of study drug or placebo given was 1g/100mL bolus followed by 1g/250mL infusion over 8 hours; normal saline was used as the placebo substance. Following the initial hospital visit, brain MRI scans were taken in two weeks. A detailed history of patients’ medical and cardiovascular history as well as demographic factors was recorded and follow up data was collected for up to 90 days. DWIHL was defined as focal hyperintense lesions on diffusion-weighted imaging and spatially remote (>20 mm) from the index lesion, as assessed by consensus between at least two of three neuroradiological experts. The locations of DWIHL were as follows: 86.6% in cerebral lobes, 5.5% within deep supratentorial grey matter, 5.5% within the cerebellum and 2.4% within the brainstem. There were no significant differences in the rate of DIWHL between the experimental and control groups; in the TXA group, 20.8% of patients had DWIHL lesions and 22.8% of the control group did. The odds ratio (OR) was 0.71 with a 95% confidence interval of 0.33 to 1.53. On subgroup analysis, cerebral amyloid angiopathy was found to significantly increase the risk of DWIHL detected on MRI study; the odds ratio was 0.34 in patients without cerebral amyloid angiopathy compared to those without (95% confidence interval 0.13-0.87). Patients who had chronic infarcts were less likely to have new DWIHL on imaging after having received TXA (odds ratio 0.19, 95% confidence interval 0.05-0.72). The increased risk of ischemic stroke within 90 days following detection of DIWHL on MRI is quantified by an absolute difference in incident rate of 9.2% (P = 0.02).
Image: PD
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.