The RAPTURE trial: Radiofrequency ablation effective and safe in lung cancer [Classics Series]
This study summary is an excerpt from the book 2 Minute Medicine’s The Classics in Medicine: Summaries of the Landmark Trials
1. Percutaneous radiofrequency ablation (RFA) demonstrated robust levels of efficacy and safety in patients with malignant lung cancers who are poor candidates for surgery.
2. RFA was only performed in lung tumors less than 3.5 cm in diameter in this cohort.
Original Date of Publication: July 2008
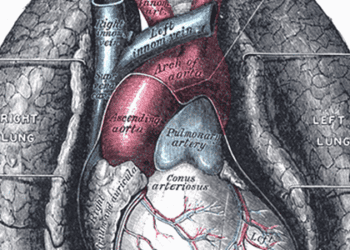
Study Rundown: Primary lung cancer is the leading cause of death in the United States with over 160 000 deaths annually. Lungs are also a frequent site of metastasis from colorectal, breast, and renal cancers. Traditional treatment of malignant lung cancers primarily involved surgical resection. However, this excluded a large group of patients with reduced pulmonary reserve or comorbid conditions who were deemed poor surgical candidates. A previous retrospective review by Simon et al. demonstrated in a cohort of 153 patients that CT-guided RFA of lung tumors were associated with robust rates of safety and promising long-term survival rates. The purpose of this landmark prospective trial was to determine the safety and efficacy of RFA in malignant lung cancers. The trial prospectively followed over 100 patients with either non-small cell lung cancer (NSCLC) or lung metastasis that was deemed ineligible for other curative treatments. The trial only included patients with up to three tumors per lung with no tumor larger than 3.5 cm in diameter. The primary outcome was technical success, safety, and confirmed response as determined by a 1 month follow-up CT scan. At the conclusion of the trial, technical success was achieved in 99% of patients with no significant changes to pulmonary function or procedure-related deaths within the study group. Complete clinical response was maintained in 88% of patients at 1 year post procedure, with no difference in responsiveness between tumor subtypes. The study is limited by the relatively small sample size and the lack of efficacy data for masses greater than 3.5 cm due to the technical size limitations of the ablation sphere. Additionally, Simons et al. and others have shown poorer clinical outcome for patients with tumor greater than 3 cm in size. Given the lack of current randomized controlled trials in this population, this was one of the first trials to demonstrate prospectively the robust technical feasibility and safety profile of RFA in the treatment of malignant lung cancers.
Click to read the study in The Lancet Oncology
In-Depth [prospective cohort]: This study was a prospective, intention-to-treat, multi-center clinical trial of 106 patients from seven centers in Europe, United States, and Australia. Patients with pathology-proven NSCLC (n = 33), or metastasis from other primary cancers (n = 73) were included. All patients were deemed a non-surgical candidate or unfit for additional radiotherapy or chemotherapy. Key exclusion criteria included patients with greater than three tumors per lung, tumor size of 3.5 cm or greater, or patients with previous pneumonectomy. RFA was performed by a 150-200 W generators with a deployment device with a maximum ablation sphere of 5 cm in diameter. Post-procedure, patients were schedule for follow-up at 3 months intervals for up to two years. The primary outcome of interest was the technical success, safety, and rate of confirmed clinical response. Clinical response was defined as a reduction in tumor size of at least 30% with no evidence of tumor growth or contrast enhancement on follow-up CT scan. Secondary outcomes were overall and cancer-specific survival. At the conclusion of the trial, technical success was achieved in 105 of 106 (99%) patients. With respect to complications, 20% of patients experienced symptomatic pneumothorax requiring chest tube drainage, however, there were no procedural-related deaths or worsening of pulmonary function performance post-RFA. Confirmed clinical response of treated lesions was demonstrated in 88% of the patient cohort. There were no differences noted in tumor response between cancer subtypes. Overall, the two-year cancer-specific survival rate for patients with NSCLC, colorectal metastases, and other primary metastases were 73% (95%CI 0.54-0.86), 68% (95%CI 0.54-0.80), and 67% (95%CI 0.48-0.84), respectively.
Lencioni R, Crocetti L, Cioni R, Suh R, Glenn D, Regge D, et al. Response to radiofrequency ablation of pulmonary tumors: a prospective, intention-to-treat, multicentre clinical trial (the RAPTURE study). Lancet Oncol. 2008 Jul;9(7):621–8.
Additional Review:
Simon CJ, Dupuy DE, DiPetrillo TA, Safran HP, Grieco CA, Ng T, et al. Pulmonary Radiofrequency Ablation: Long-term Safety and Efficacy in 153 Patients. Radiology. 2007 Apr 1;243(1):268–75.
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.




![The ABCD2 score: Risk of stroke after Transient Ischemic Attack (TIA) [Classics Series]](https://www.2minutemedicine.com/wp-content/uploads/2013/05/web-cover-classics-with-logo-medicine-BW-small-jpg-75x75.jpg)