Initial dexamethasone improves long-term survival in acute bacterial meningitis
[tabs tab1=”2MM Rundown” tab2= “Full 2MM Report” tab3=”About the Authors”]
[tab]
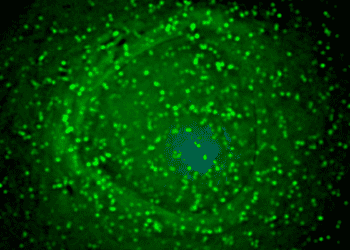
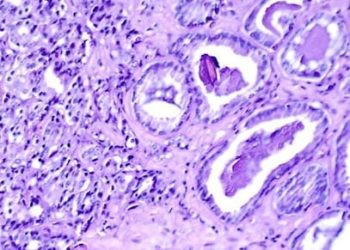
Image: PD/CDC. S.Pneumo
1. Adjunctive dexamethasone has previously been shown to improve short-term survival in acute bacterial meningitis.
2. The improved survival effect remains significant up to fifteen years after initial infection.
Adjunctive dexamethasone in the treatment of acute bacterial meningitis is known to increase survival in the early post-infection period. In the present study, the authors demonstrated the lasting effect of this survival benefit. This effect was particularly strong in cases of meningitis due to Streptococcus pneumoniae. Of note, as the patients in the 2002 study were recruited over nine years, the authors were able to determine mortality up to nineteen years after infection.
This study is limited by the lack of data on the effect of dexamethasone on meningitis due to other common causative organisms, which prevents a comparison between the strong survival benefit in Streptococcus pneumoniae cases with other pathogens such as Neisseria meningitidis. Additionally, the authors focus only on survival and do not explore the potential long-term benefit of dexamethasone on other neurologic sequelae; that said, no short-term benefits on these outcomes were found in the original study. Regardless, the authors’ present findings accentuate the benefit of dexamethasone in the empiric treatment of acute bacterial meningitis.
Click to read the study in Neurology (early release)
[/tab]
[tab]
Image: PD/CDC. S.Pneumo
1. Adjunctive dexamethasone has previously been shown to improve short-term survival in acute bacterial meningitis.
2. The improved survival effect remains significant up to fifteen years after initial infection.
Primer: Meningitis, or inflammation of the coverings of the brain and spinal cord (the meninges), is a life-threatening condition with a 10-20% mortality. Though the incidence in the United States has declined over fifty percent in the last few decades, it remains relatively common at 1.3-2 per 100,000 annually (1). The bacterium Streptococcus pneumoniae is the most common cause, followed by Neisseria meningitidis (primarily in younger patients) and Listeria monocytogenes. Viruses and fungi are less commonly responsible. In patients surviving initial infection, long-term sequelae may include hearing loss, cognitive impairment, increased risk of epilepsy, and other various neurologic consequences.
Wide-spectrum antibiotics have long been the mainstay of empiric treatment. In 2002, a landmark paper was published based on the European Dexamethasone in Adulthood Bacterial Meningitis Study. In it, the authors reported a beneficial effect of adjunctive corticosteroids given prior to the first dose of empiric antibiotics. Specifically, overall mortality was decreased and Glasgow Outcome Scale scores were higher at 8 weeks post-infection (2). As a result, administration of ten milligrams dexamethasone every six hours for the first four days of therapy has become the new standard of care in the United States and other high-income countries (3). In the present study, the authors of the study analyzed long-term follow-up of the initial cohort to determine the effect of adjunctive dexamethasone on long-term survival.
Background reading:
- Acute community-acquired bacterial meningitis in adults: An evidence-based review
- Dexamethasone in adults with bacterial meningitis
- Advances in treatment of bacterial meningitis
This [cohort] study: In the initial 2002 study, 144 patients randomized to antibiotics and dexamethasone at the dosage described above were compared to 157 controls receiving antibiotics only. Of these, 228 patients were available for the current analysis. All together, there have been 31 total deaths (22%) in the steroid group in comparison to 44 deaths (33%) in the antibiotic only group. While the mortality after the initial study period was not significantly different (p=0.27), the proportional overall survival in patients receiving dexamethasone was significantly higher (p=0.029). This effect was strongest in patients initially infected with Streptococcus pneumoniae (p=0.009). Age was the only predictor of death after the initial 8 week post-infectious period. Moreover, individual patient survival was not correlated with their Glasgow Outcome Score at 8 weeks after infection.
In sum: Adjunctive dexamethasone in the treatment of acute bacterial meningitis is known to increase survival in the early post-infection period. In the present study, the authors demonstrated the lasting effect of this survival benefit. This effect was particularly strong in cases of meningitis due to Streptococcus pneumoniae. Of note, as the patients in the 2002 study were recruited over nine years, the authors were able to determine mortality up to nineteen years after infection.
This study is limited by the lack of data on the effect of dexamethasone on meningitis due to other common causative organisms, which prevents a comparison between the strong survival benefit in Streptococcus pneumoniae cases with other pathogens such as Neisseria meningitidis. Additionally, the authors focus only on survival and do not explore the potential long-term benefit of dexamethasone on other neurologic sequelae; that said, no short-term benefits on these outcomes were found in the original study. Regardless, the authors’ present findings accentuate the benefit of dexamethasone in the empiric treatment of acute bacterial meningitis.
Click to read the study in Neurology (early release)
By [JD] and [RR]
© 2012 2minutemedicine.com. All rights reserved. No works may be reproduced without written consent from 2minutemedicine.com. Disclaimer: We present factual information directly from peer reviewed medical journals. No post should be construed as medical advice and is not intended as such by the authors or by 2minutemedicine.com. PLEASE SEE A HEALTHCARE PROVIDER IN YOUR AREA IF YOU SEEK MEDICAL ADVICE OF ANY SORT.
[/tab]
[tab]

John Prendergass: John is a 2nd year M.D. candidate at New Jersey Medical School. He was raised in Jersey City, NJ and attended Johns Hopkins University for his undergraduate degree in Behavioral Biology. His academic interests include general surgery, neuroscience, and pediatrics. Outside of school John enjoys basketball and soccer.
 Rif Rahman: Rif is a 4th year M.D. candidate at Harvard Medical School, currently completing a research year investigating the use of conventional and advanced imaging techniques to assess treatment response of high grade gliomas. His medical interests are in the areas of internal medicine and neurology.
Rif Rahman: Rif is a 4th year M.D. candidate at Harvard Medical School, currently completing a research year investigating the use of conventional and advanced imaging techniques to assess treatment response of high grade gliomas. His medical interests are in the areas of internal medicine and neurology.
[/tab]
[/tabs]