PET imaging findings may precede cognitive impairment in patients at high risk for Alzheimer’s disease
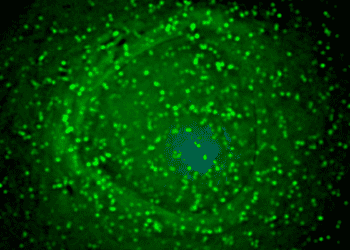
Image: PD
Key study points:
- PET imaging changes can be detected in the posterior cingulate cortex prior to hippocampal changes in adults without cognitive impairment.
- These changes in PET imaging are more prevalent in patients with APOEε4 allele carriers, who are genetically at increased risk of Alzheimer’s Disease, in a dose-dependent manner.
Primer: Alzheimer’s disease (AD) is the most common form of dementia, estimated to affect nearly thirty million people worldwide. The majority of cases occur in persons older than 65, beginning with minor anterograde memory deficits and progression over years to complete dependence on caregivers and eventually death from secondary illness. Pathologically, AD is characterized by loss of cholinergic neurons in the nucleus basalis of Meynert, as well as accumulation of beta-amyloid and neurofibrillary tangles in various regions throughout the brain. While most cases of AD are sporadic, the apolipoprotein E (APOE) gene has been implicated as a genetic risk factor in a dose-dependent manner; the APOEε4 allele confers a three- and fifteen-fold risk of developing AD in heterozygotes and homozygotes, respectively.
Structural imaging (traditional MRI) has been the most commonly used method to track the pathologic changes in AD. Using this method, studies have identified significant atrophy of the hippocampal and entorhinal cortices that corresponds to early cognitive changes in patients with AD, followed by ventricular and sulcal enlargement, grey matter atrophy, and reduced cortical thickness. More recently, positron emission tomography (PET) imaging, which uses radiolabeled glucose to assess regional brain metabolic activity, has demonstrated decreased glucose metabolism in the hippocampus in conjunction with atrophy and clinical symptoms. In the present study, the authors examined hippocampal atrophy and metabolism, as well as the metabolism in the functionally related posterior cingulate cortex, relative to APOEε4 carrier status and clinical status in adults without cognitive dysfunction, in order to determine the relationship between early brain alterations and risk of AD in later life.
Background reading:
This [cross-sectional] study: The authors examined 149 cognitively normal adults, aged 49 to 67, without psychiatric disease, cardiovascular disease, or abnormal neurologic findings. All participants received structural MRI and PET scans and were genotyped to determine APOEε4 carrier status. Patients were stratified into non-carrier, heterozygote, and homozygote groups for analysis. No significant differences were found across groups for age, education, or performance on neuropsychological testing. Hippocampal volumes and glucose metabolism were not significantly different across the three groups, nor was there a significant downward linear trend based on APOEε4 dose. However, carriers of the APOEε4 allele showed significantly decreased glucose metabolism in the cingulate cortex, with a significant APOEε4 dose-dependent downward trend.
In sum: This study demonstrates that a reduction in posterior cingulate cortex glucose metabolism precedes the development of cognitive dysfunction in adults at risk for Alzheimer’s disease. This effect was greatest in participants homozygous for the APOEε4 allele, who are considered to be at highest risk for later AD. These changes preceded atrophy or reduced glucose metabolism in the hippocampus, which has long been the primary neuroimaging biomarker in AD.
Given the tremendous disease burden of AD, the identification of a non-invasive predictive biomarker would be incredibly valuable. Nonetheless, the results of this study should not be over-interpreted, as reduced cingulate metabolism may only be coincidentally associated with APOEε4 rather than a feature of AD pathology, and may not actually predict development of clinical disease. Moreover, these findings have yet to be correlated with other neuroimaging measures of AD pathology, and they will need to be tracked over the course of the disease to determine their true relationship to AD progression. Nonetheless, the authors have demonstrated a potentially important non-invasive biomarker for increased AD risk that warrants continued investigation.
Click to read the study in Archives of Neurology
Click to read an accompanying editorial in Archives of Neurology
By [JD] and [RR]
More from this author: Initial dexamethasone improves long-term survival in acute bacterial meningitis, Elevated systolic blood pressure linked to white matter brain damage in young adults, Retired NFL players are at increased risk of death due to neurodegenerative disease, Asymptomatic carotid stenosis increases risk for cognitive dysfunction
© 2012 2minutemedicine.com. All rights reserved. No works may be reproduced without written consent from 2minutemedicine.com. Disclaimer: We present factual information directly from peer reviewed medical journals. No post should be construed as medical advice and is not intended as such by the authors or by 2minutemedicine.com. PLEASE SEE A HEALTHCARE PROVIDER IN YOUR AREA IF YOU SEEK MEDICAL ADVICE OF ANY SORT.