2 Minute Medicine Rewind November 13, 2023
mRNA SARS-CoV-2 Vaccination Before vs During Pregnancy and Omicron Infection Among Infants
1. In a retrospective cohort of Singaporean, maternal mRNA SARS-CoV-2 vaccination during pregnancy was associated with a 41.5% reduction in SaR-CoV-2 infection for infants aged 6 months or less.
2. Vaccination during pregnancy demonstrated a larger risk reduction for infants than vaccinations administered prior to pregnancy.
Evidence Rating Level: 2 (Good)
Analysis of population data suggests that infants aged 6 months or younger face an increased risk of severe SARS-CoV-2 infection compared to other age groups, representing a significant portion of COVID-19 hospitalizations during the Omicron-dominant waves. Maternal vaccination has been proposed as a preventative measure to prevent severe infections in newborns, though there continues to be a scarcity of evidence examining the optimal timing of vaccination and its efficacy in preventing severe Omicron XBB variant COVID-19 infections. This retrospective cohort study, spanning January 1, 2022, to March 31, 2023, sourced information from the official Singapore Ministry of Health databases to investigate this knowledge gap, specifically identifying infants up to 6 months of age. Maternal vaccination status was categorized into unvaccinated, vaccinated prior to pregnancy, and vaccinated during pregnancy. Inverse probability weighting addressed confounding factors, and Cox regressions estimated hazard ratios of SARS-CoV-2 infections and a vaccine effectiveness (VE) score was also calculated. Of 7,292 infants, maternal mRNA SARS-CoV-2 vaccination during pregnancy was associated with a 41.5% (95% CI, 22.8%-55.7%) reduction in SARS-CoV-2 infection risk. Notably, vaccination including a third dose (booster) during pregnancy demonstrated a significant 44.4% (95% CI, 26.2%-58.1%) VE, while vaccination prior to pregnancy showed only a 15.4% (95% CI, −17.6% to 39.1%) reduction. Infants born to mothers who received a third dose (booster) during pregnancy exhibited a VE of 76.7% (95% CI, 12.8%-93.8%) against the Omicron XBB variant. Notably however, the study was limited in that it did not analyze breastfeeding data, and hospitalization guidelines during the study period varied throughout. Nonetheless, there appears to be a protective impact of maternal mRNA SARS-CoV-2 vaccination during pregnancy to prevent severe Omicron XBB variant COVID-19 infections. This may help further inform prenatal vaccination counseling to optimize protection for newborns.
Perceived Interpersonal Racism and Incident Stroke Among US Black Women
1. In this cohort study, a 38% increased risk of stroke was reported amongst black women reporting interpersonal racism in employment, housing, and police interactions.
Evidence Rating Level: 2 (Good)
It is well documented in prior literature that black individuals in the United States face disproportionately higher stroke incidence and mortality rates compared to their White counterparts. This association is most marked in black women, who experience the highest rates and earliest onset of stroke compared to women from other racial groups. Although social determinants of health have been used to determine potential causes of this discrepancy, there has been a lack of literature directly examining the association of interpersonal racism and stroke incidence. The study, conducted within the Black Women’s Health Study (BWHS), initiated in 1995, a prospective cohort study that encompassed 48,375 participants. Participants aged 21-69 at baseline during the study period provided detailed health and psychosocial information through questionnaires and were followed up through 2019. This cohort study sought to identify stroke cases that were gathered through the BWHS questionnaires and medical records review, and characterize their association with perceived interpersonal racism using questions focused on interactions in everyday life and in the workplace, housing market, and with law enforcement. During follow-up from 1997 through 2019, 1664 incident strokes were identified. Women in the highest quartile of perceived interpersonal racism in everyday life had an age-adjusted HR for stroke of 1.28. The multivariable HR was 1.14. For those experiencing racism in employment, housing, and police, the age-adjusted HR for stroke was 1.42, with a multivariable HR of 1.38. Study findings suggest that independent of other risk factors such as smoking, age, etc., the experience of interpersonal racism was associated with a significantly increased stroke risk. Although future studies will be required given the complexities of racism and racial discrimination, findings underscore the significance of racism itself as a social determinant of health and its contribution to stroke risk.
1. In a large population-based cohort study, combination therapy of antidepressant therapy with a statin was associated with fewer antidepressant treatment discontinuations.
2. Augmentation of antidepressant therapy with a statin was not associated with any differences in treatment efficacy.
Evidence Rating Level: 2 (Good)
Antidepressants, while effective at treating depression, are often discontinued due to treatment intolerance. There has been recent interest in the exploration of adjunctive medication options to improve treatment tolerance, with statins being proposed as one of these agents. In this population-based cohort study, data from the QResearch registry of 673,177 patients with depression was analyzed to determine if there would be lower rates of discontinuation with combination therapy. The study additionally examined changes on Patient Health Questionnaire (PHQ)-9 scores to determine if combination therapy would be associated with differences in treatment efficacy. In the cohort, 46,482 patients received antidepressant + statin, while 626,335 received antidepressant-only. The results revealed that the combination therapy was associated with reduced antidepressant discontinuations at 2, 6, and 12 months. However, no significant differences were observed in efficacy outcomes measured using the Patient Health Questionnaire (PHQ)-9. Overall, combination therapy with antidepressants and statins appeared to improve the acceptability of antidepressant treatment. Further research will be required prior to making this a standard of care however unless otherwise clinically indicated, especially given no statistical differences in treatment response and the mechanism of the effect remaining unknown. Nonetheless, this study does appear to corroborate prior evidence suggesting a potential role for adjunctive medications to decrease antidepressant discontinuations in the future.
1. For individuals over age 50 who received the live zoster vaccine, protection against herpes zoster, postherpetic neuralgia, herpes zoster opthalmicus, and hospital admissions was strongest in the first year and waned substantially over the follow-up period.
Evidence Rating Level: 1 (Excellent)
Herpes zoster (HZ) is the virus responsible for shingles, a painful rash that can develop in anyone previously infected with varicella zoster. Complications of HZ include postherpetic neuralgia and herpes zoster opthalmicus, with few patients requiring hospital admission. This prospective cohort study aimed to assess the vaccine’s effectiveness in preventing HZ and its complications within 10 years of immunization. The study was conducted by analyzing the electronic health records of 1,505,647 individuals over age 50 between January 2007 and December 2018. All individuals were unvaccinated for HZ at the start of the study period. Of this cohort, 34% of participants were vaccinated with the live zoster vaccine. Over the follow-up period, there were 75,135 incident HZ cases, of which 7% developed postherpetic neuralgia, 6% developed herpes zoster opthalmicus, and 0.7% required hospital admission. For all of these outcomes, the effectiveness of the vaccine was greatest in the first year after immunization but decreased over time. For protection against herpes zoster, the vaccine’s effectiveness decreased from 67% (95% CI, 65%-69%) in the first year to 15% (5%-24%) at 10 years. For protection against postherpetic neuralgia, the vaccine’s effectiveness decreased from 83% (78%-87%) to 41% (17%-59%) over 10 years. Similar trends were observed for herpes zoster opthalmicus and hospital admissions. A limitation of this study is that the researchers required the presence of both a diagnosis and antiviral prescription to count a case of HZ, and as such, the number of incident cases may have been underrepresented. Overall, this study demonstrates that the live zoster vaccine was effective in preventing HZ and its complications, but the protection waned substantially over the 10-year follow-up period.
1. In this retrospective population-based study, vaccination against COVID-19 among those over age 50 in France was effective in reducing morbidity, mortality, and stress on the healthcare system.
Evidence Rating Level: 2 (Good)
Following the widespread distribution of vaccines against COVID-19, it is important to retrospectively evaluate the effectiveness of this public health endeavor. Researchers aimed to assess the number of COVID-19-related hospitalizations, ICU admissions, and deaths that were avoided by vaccination in France. This retrospective ecological study utilized French national surveillance data on individuals over age 50 from December 28, 2020 to March 6, 2022. 279,443 hospitalizations, 60,186 ICU admissions, and 74,690 deaths occurred due to COVID-19 during the study period. In total, 25,152,788 individuals over age 50 received at least one dose of a vaccine against COVID-19. Researchers estimated that 480,150 (95% CI, 260,072-582,516) hospitalizations, 132,156 (95% CI, 50,409-157,767) ICU admissions, and 125,376 (95% CI, 53,792-152,037) deaths among those over the age of 50 were prevented by vaccination. A limitation of this study is that only data on deaths reported by hospitals and nursing homes were included, and as such, no deaths that occurred in other settings were accounted for, such as deaths at home. As well, this study appropriately addressed the benefits of vaccination for those who received the vaccine, but future studies may assess the effects of vaccination on herd immunity and protecting unvaccinated members of the population as well. Overall, this study demonstrates that vaccination against COVID-19 was an effective strategy for reducing morbidity and mortality, as well as lessening the strain on the healthcare system in France.
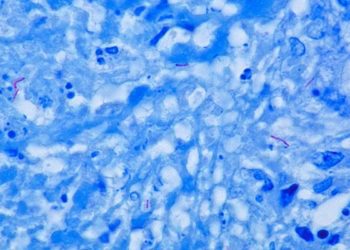
Image: PD
©2023 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.