Capecitabine or XELOX did not appear to improve overall survival when compared to PF in patients with advanced Esophageal Squamous Cell Carcinoma
1. Although capecitabine or XELOX did not improve overall survival when compared to PF, efficacy was comparable suggesting single-agent capecitabine as a potential alternative to combination chemotherapy for select patients.
2. Single-agent capecitabine showed a lower rate of grade 3 adverse events when compared to PF or XELOX.
Evidence Rating Level: 1 (Excellent)
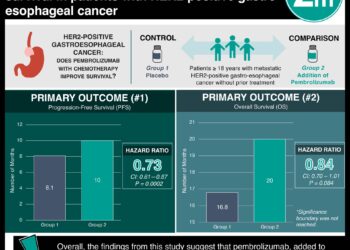
Study Rundown: In this phase 3, randomized trial, 246 patients with inoperable, locally advanced esophageal squamous cell carcinoma (ESCC) were assigned to one of three treatment arms: capecitabine, XELOX (capecitabine + oxaliplatin), or PF (cisplatin + fluorouracil). Patients in each treatment arm were then again, randomly assigned to receive consolidation chemotherapy (with the same treatment regimen) or not. All patients received radiation therapy. The primary endpoints were the 2-year overall survival (OS) rate and incidence of grade 3 adverse events (AE). The secondary endpoints were progression-free survival (PFS) and clinical complete response (CCR). This study suggests that, although efficacy was comparable, capecitabine or XELOX did not significantly improve the 2-year OS rate, when compared to PF; single-agent capecitabine did have a lower incidence of grade 3 AE’s than PF, suggesting capecitabine as a potential alternative treatment option for select patients with locally advanced ESCC. Limitations of this study include the small sample size, as well as the patient population, which included primarily Chinese patients who had never smoked or consumed alcohol, making application to Western patients with ESCC limited.
Click to read the study in JCO
Relevant Reading: Chemoradiotherapy of Locally Advanced Esophageal Cancer
In-Depth [randomized controlled trial]: In this trial, 246 patients with locally advanced, inoperable ESCC were assigned to receive 2 cycles of either capecitabine (n=80), XELOX (n=85) or PF (n=81). Half of the patients, in each treatment arm, received consolidation chemotherapy (n=38 for the capecitabine group, n=43 for XELOX group, n=37 for PF group). The median follow-up time was 33.6 months. In the capecitabine arm, the 2-year OS rate was 75% (capecitabine v PF: HR 0.91 [95% CI, 0.61 to 1.35], nominal P = .637), the median PFS was 26.1 months (95% CI, 18.4 to 31.8), and 35% of patients achieved a CCR. In the XELOX arm, the 2-year OS rate was 66.7% (XELOX vs PF: HR, 0.86 [95% CI 0.58 to 1.27]; P = .444), the median PFS was 30.2 months (95% CI, 15.9 to 39.6), and 37.6% of patients achieved a CCR. In the PF arm, the 2-year OS rate was 70.9%, the median PFS was 28.2 months (95% CI, 16.6 to 34.9), and 33.3% achieved a CCR. For the consolidation chemotherapy group, the 2-year OS rate was 75.6% and the median PFS was 30.7 months; for the non-consolidation chemotherapy group, the 2-year OS rate was only 66.3% and the median PFS was 24.9 months. For grade 3 AE’s, 28.8% of patients in the capecitabine group, 36.5% of patients in the XEOLX group, and 45.7% of patients in the PF group experienced grade 3 AEs throughout the study, with pneumonitis being the most common grade 3 AE in each treatment group. Ultimately, although this study did not show that capecitabine or XELOX improved the 2-year OS rate, compared to PF, it did suggest similar efficacy amongst the 3 treatment groups, goes on to suggest that consolidation chemotherapy may improve outcomes, and suggests that single-agent capecitabine has an improved tolerability profile so could be considered for select patients with inoperable, locally advanced ESCC.
Image: PD
©2024 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.