Hyperthermic intraperitoneal chemotherapy may be less risky than expected
Image: PD
1. Hyperthermic intraperitoneal chemotherapy (HIPEC) following cytoreductive surgery had a 2% 30-day mortality.
2. Large prospective trials are necessary to confirm the role of HIPEC in the modern therapeutic regimen.
Evidence Rating Level: 2 (Good)
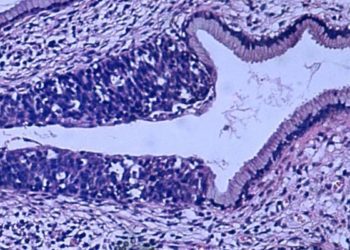
Study Rundown: The management of peritoneal carcinomatosis is split between systemic and HIPEC. HIPEC allows the administration of locally high concentrations of therapeutic agent in combination with temperatures cytotoxic to malignant cells. It has been demonstrated that surgery combined with HIPEC can improve long-term survival in carefully selected colorectal, appendiceal, and primary peritoneal cancer patients with good performance status and low volume of peritoneal disease. However, it is a complicated procedure with a lack of evidence demonstrating its superiority over systemic chemo making it an uncommon choice of treatment. This study set out to report morbidity and mortality data on a large set of HIPEC patients, and found an overall 30-day morbidity and mortality of 33% and 2%, respectively. However, this study’s results may have been swayed by greater expertise in participating hospitals than available nationwide. While the low 30-day mortality is a convincing indicator that treatment-associated deaths are within acceptable limits, prospective trials with longer-term follow-up are necessary to confirm the safety and efficacy of HIPEC.
Click to read the study in JAMA Surgery
Relevant Reading: Intraperitoneal chemotherapy: Rationale, applications, and limitations
In-Depth [retrospective cohort]: A total of 694 HIPEC cases with cytoreductive procedures occurring 2005-2011 were culled from the American College of Surgeons National Surgical Quality Improvement Program database. Primary endpoints were overall 30-day mortality and morbidity. Patient and treatment characteristics were used to build predictive models for respiratory complications, septic shock, and return to the OR based on the Lasso algorithm. Appendiceal cancer was present in 14% of patients, primary peritoneal in 11%, and colorectal cancer in 8%. Overall mortality was 2.3%, mostly after post-op day 17, and 9.8% of patients returned to the OR. Postoperative bleeding requiring transfusion occurred in 17% of patients, septic shock in 16%, pulmonary complications in 15%, and organ-space infections in 9% of patients. Analysis failed to identify any strong predictors of morbidity or mortality.
By Mariya Samoylova and Allen Ho
More from this author: Resident involvement linked with more complications in joint surgery; Promising liver transplant outcomes at 20 years; Transfusion worsens outcomes for HCV+ liver transplant recipients; Endovascular repair of ruptured AAAs no better than open repair ; Longer preoperative treatment of pancreatic cancer may extend survival
©2012-2013 2minutemedicine.com. All rights reserved. No works may be reproduced without expressed written consent from 2minutemedicine.com. Disclaimer: We present factual information directly from peer reviewed medical journals. No post should be construed as medical advice and is not intended as such by the authors, editors, staff or by 2minutemedicine.com. PLEASE SEE A HEALTHCARE PROVIDER IN YOUR AREA IF YOU SEEK MEDICAL ADVICE OF ANY SORT.