Adjuvant celecoxib not associated with improved disease-free survival in patients with ERBB2-negative breast cancer
1. The study found no evidence of benefit to disease-free survival when 400 mg of celecoxib was administered once daily for 2 years in patients with ERBB2-negative breast cancer as compared to the placebo group.
2. Due to gastrointestinal and cardiac adverse effects related to COX-2 inhibition, longer-term treatment or tolerable use of a greater dose of celecoxib may be needed to achieve clinical benefit, highlighting the need for further studies.
Evidence Rating Level: 1 (Excellent)
Study Rundown: It has been well established that patients with breast cancer often remain at risk of relapse after conventional adjuvant therapy. More recently, preliminary results on celecoxib, a COX-2 inhibitor and nonsteroidal anti-inflammatory drug (NSAID), has shown promising antitumor activity in preclinical models of human breast cancer where strong clinical evidence is still lacking. In view of these preclinical results, the International Collaborative Cancer Group (ICCG) and the German Breast Group (GBG) initiated a trial to evaluate the role and effect on disease outcomes of adjuvant celecoxib with conventional therapy in women with ERBB2 (formerly HER2)-negative primary breast cancer. An emphasis was placed on the collection of data on gastrointestinal and cardiac adverse events with a focus on women without cardiovascular risk factors due to adverse effects reported with long-term celecoxib therapy. The main outcome and measure of the analysis was disease-free survival (DFS), assessed in the intention-to-treat population via Cox proportional hazards regression and log-rank analysis. From 2,639 patients randomized 2:1 to receive treatment with celecoxib or placebo for 2 years, DFS events were reported for 487 total patients (19%), where 323 (18%) of those receiving celecoxib reported a 5-year DFS rate of 84% and 164 (19%) of those receiving placebo reported a 5-year DFS rate of 83%, a nonsignificant statistical difference. Thus, despite preclinical evidence suggesting that COX-2 inhibitors were associated with improved disease outcomes in patients with early breast cancer, this randomized clinical trial found no evidence of benefit when 400 mg of celecoxib was administered once daily for 2 years to patients with ERBB2-negative breast cancer. A limitation of this study was that in several patients experiencing cardiac adverse events, the dose of celecoxib was reduced. Thus, the study was unable to exclude the possibility that a higher dose of celecoxib may result in improved outcomes.
Click to read the study in JAMA Oncology
Click to read an accompanying editorial in JAMA Oncology
Relevant Reading: Elevated expression of cyclooxygenase-2 is a negative prognostic factor for disease free survival and overall survival in patients with breast carcinoma
In-Depth [randomized controlled trial]: The Randomized European Celecoxib Trial (REACT) was a phase 3, randomized, double-blind study conducted across 160 centers in the UK and Germany where 2,639 patients (median age, 55.2 years [range, 26.8-86.0 years]) were recruited. In a 2:1 randomization ratio, 1,763 patients received 400 mg of celecoxib once daily and 876 patients received the placebo regimen for 2 years total. Data was collected between January 2007 and November 2012 with follow-up for 10 years (median follow-up [IQR], 74.3 [61.4-93.6] months) after treatment completion and statistical analysis completed in March 2020. Inclusion criteria included patients who had completely resected breast cancer with local and systemic therapy as per local practice guidelines. Exclusion criteria included patients with ERBB2-positive or node-negative and T1, grade 1 tumors. In total, 1,930 patients (73%) had estrogen receptor positive or progesterone receptor positive and ERBB2 negative tumors, 1,265 (48%) had node-positive disease, and 1,111 (42%) had grade 3 tumors. Upon follow-up, DFS data was available for 487 (19%) patients where the unadjusted hazard ratio was 0.97 (95%CI, 0.80-1.17; log-rank P = .75). Of 1,763 patients who originally received celecoxib, follow-up data on 323 (18%) patients had a 5-year DFS rate of 84%. Of 876 patients who originally received placebo, follow-up data on 164 (19%) individuals had a 5-year DFS rate of 83%. Lastly, rates of toxic effects were low across both the celecoxib and placebo cohorts, with no evidence of a significant difference.
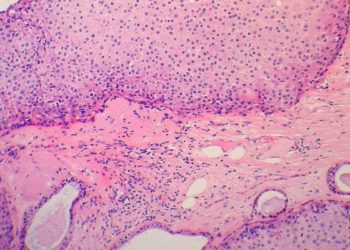
Image: PD
©2021 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.