Adjuvant dexamethasone improves outcomes in adult bacterial meningitis [Classics Series]
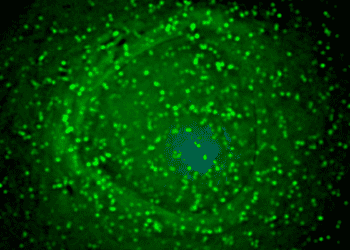
Image: CC/L. academia
1. Treatment with dexamethasone reduces morbidity and mortality in adults with bacterial meningitis
2. There is no significant difference in risk of adverse events with corticosteroid treatment
Original Date of Publication: November 14, 2002
Study Rundown: The results of this study show that early adjuvant dexamethasone (10 mg every six hours for four days) reduces morbidity and mortality in adults with acute bacterial meningitis. The beneficial effect of dexamethasone was clear in patients with pneumococcal meningitis but a significant benefit was not shown in patients with meningococcal meningitis, possibly due to the limited number of patients in this subgroup. There was some concern regarding delay in treatment initiation due to informed-consent procedures and the time required for cranial CT and lumbar puncture when it was indicated for patients. Previous studies have suggested that two- and four-day regimens of dexamethasone therapy are equally effective. This study used and recommends a four-day regimen, initiated before or with the first dose of antibiotics.
There is concern that dexamethasone reduces the permeability of the blood-brain barrier limiting the penetration of vancomycin, which is used increasingly for penicillin-resistant pneumococci. Thus, patients receiving vancomycin and dexamethasone should be carefully observed. Although the reduction in mortality in this study was not associated with a higher rate of neurologic sequelae, corticosteroids may be associated with ischemic injury to neurons and so further research should investigate cognitive impairment in adults treated with and without dexamethasone.
In sum, this trial calls for the early administration of dexamethasone along with antibiotic therapy in adult patients with bacterial meningitis, as treatment with adjuvant dexamethasone was shown to reduce morbidity and mortality.
Primer: Bacterial meningitis is a neurological emergency with high fatality rates and results in neurologic deficits in nearly a third of survivors. Streptococcus pneumoniae and Neisseria meningitidis are the most common causes of bacterial meningitis, accounting for 80% of adult cases. Pneumococcal meningitis refers to infection caused by S. pneumoniae while meningococcal meningitis refers to infection by N. meningitidis. Bacterial meningitis is suspected in patients presenting with the classic triad of fever, neck stiffness and altered mental status. The triad has a low sensitivity but almost all patients present with at least two of four symptoms: headache, fever, neck stiffness and altered mental status. Culture and stain of a cerebrospinal fluid obtained by lumbar puncture is the definitive method of diagnosis and identification of the etiologic agent. However, there is a significant risk of brain herniation with the lumbar puncture due to high cranial pressure and so neuroimaging, normally by cranial computed tomography (CT) is recommended before lumbar puncture to detect brain shift.
Antibiotic therapy should be initiated as soon as possible. Third-generation cephalosporins are a standard treatment and vancomycin should be added to the regimen in cases of penicillin resistance. Adjuvant dexamethasone therapy has been shown to reduce mortality and morbidity in both children and adults with bacterial meningitis. The following study, published in NEJM in 2002, contributed to the evidence supporting the use corticosteroids to reduce inflammation and improve outcomes in cases of bacterial meningitis.
Relevant Reading:
- EFNS guideline on the management of community-acquired bacterial meningitis: Report of an EFNS Task Force on acute bacterial meningitis in older children and adults.
- Community-acquired bacterial meningitis in adults.
In-Depth [randomized, controlled study]: In this randomized, controlled trial, 301 patients with suspected meningitis were randomly assigned to receive dexamethasone or placebo along with usual antibiotic therapy. Patients in the dexamethasone group were less likely to experience an unfavourable outcome than patients in the placebo group at eight weeks after enrollment. Mortality was also lower in the dexamethasone group than the placebo group. Dexamethasone did not significantly improve or worsen neurologic sequelae (e.g. hearing loss) in survivors. Patients receiving dexamethasone were less likely to develop impaired consciousness and were less likely to have seizures or cardiorespiratory failure.
By Adrienne Cheung, Andrew Cheung, M.D.
© 2013 2minutemedicine.com. All rights reserved. No works may be reproduced without written consent from 2minutemedicine.com. Disclaimer: We present factual information directly from peer reviewed medical journals. No post should be construed as medical advice and is not intended as such by the authors or by 2minutemedicine.com. PLEASE SEE A HEALTHCARE PROVIDER IN YOUR AREA IF YOU SEEK MEDICAL ADVICE OF ANY SORT. Content is produced in accordance with fair use copyrights solely and strictly for the purpose of teaching, news and criticism. No benefit, monetary or otherwise, is realized by any participants or the owner of this domain.