Advanced care planning intervention for patients with advanced lung or colorectal cancer
1. An advanced care planning (ACP) intervention was not found to increase quality of life compared to usual care, in patients with advanced lung or colorectal cancer.
2. ACP was found to increase the number of patients receiving specialized palliative care, and having advanced directives recorded in hospital files.
Evidence Rating Level: 1 (Excellent)
Discussions regarding end-of-life plans among patients, family, and healthcare professionals are associated with numerous positive outcomes, such as better emotional functioning, increased symptom resolution, and less demanding interventions. Advanced care planning (ACP) encompasses these discussions, and allows patients to outline their goals of care, keep a record of these goals, and identify decision makers on their behalf. Although ACP has been shown to increase patient conversations, there is limited and conflicting evidence on improvements in quality of life. Therefore, this 6-country, multi-centre randomized controlled trial examined the effects of ACP on quality of life outcomes, namely emotional function and advanced cancer symptoms. The study was conducted at 23 hospitals spread throughout Belgium, Denmark, Italy, the Netherlands, Slovenia, and Great Britain. The study population consisted of 1,130 patients with advanced lung or colorectal cancer, with 685 in the control group and 445 in the intervention: Hospitals were randomized into groups, instead of individual patients. The intervention group patients had conversations with physicians certified in ACP, and also received ACP leaflets. The control group had no changes made to their hospital’s usual care protocol. The results showed that overall quality of life was not different between the intervention and control groups, with both follow-up assessments having lower quality of life scores than at baseline (for the 11-12 week follow-up: T-score -5.7, 95% CI -14.4 to 2.9 for intervention; T-score -2.0, 95% CI -4.0 to 0.1 for control; p = 0.22). There were also no differences found for coping, health symptoms, patient satisfaction, and shared decision-making. However, the intervention group received specialist palliative care more frequently (37% versus 27%, p = 0.002) and had more advanced directives included in medical files (10% versus 3%, p < 0.001). In conclusion, this study found no evidence that ACP interventions improved quality of life in advanced lung or colorectal cancer patients, which may be a testament to the strengths of usual end-of-life care, but it also has implications for examining other end-of-life approaches that can improve quality of life.
Click to read the study in PLOS Medicine
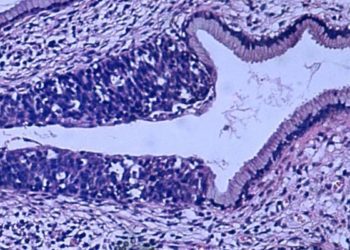
Image: PD
©2020 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.