Annual CT safe and effective for screening of nonsolid lung nodules
1. In patients with nonsolid lung nodules, yearly computed tomography (CT) scans may be used to safely screen for malignant progression regardless of lesion size.
2. Newly identified nonsolid nodules were more likely to resolve or to decrease in size than other nodules, and those that do persist and progress are likely early stage adenocarcinomas.
Evidence Rating Level: 2 (Good)
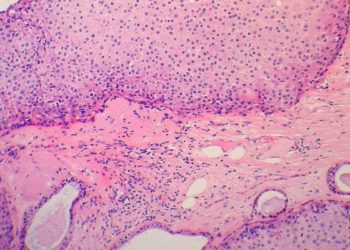
Study Rundown: The widespread utilization of chest CT scans has increased the importance of the accurate evaluation of lung nodules. These small parenchymal lesions are classified as solid, partially solid or nonsolid based on CT morphology, with solid nodules most strongly associated with malignancy. Nonsolid nodules present the most difficult assessment challenge due to their irregular morphology and poorly defined borders affecting the radiologist’s ability to quantify size over time. Typical evaluation of nonsolid nodules involves tracking them over time for potential transition to solid nodules, requiring repeated chest CT scans or invasive biopsies. The goal of this study was to examine the impact of annual CT scans on the long-term clinical course of patients with non-solid nodules. To this end, all study participants received baseline and repeated CT scans at 12-month intervals and the prevalence of nonsolid nodules was recorded, as were long-term outcomes and interventions for patients in the cohort. Prospective baseline imaging revealed that only 4.2% of patients had at least one nonsolid nodule, and only 0.7% of annual repeat screenings identified nonsolid nodules. Of these, 1/30 to 1/50 proved to be stage I adenocarcinomas, with no later stage malignancies revealed. Survival among patients with cancers identified in this fashion was 100%, therefore the authors concluded that nonsolid nodules of any size can be safely monitored with yearly CT scans. This study was limited in that not all the nonsolid nodules were readily diagnosable within the follow-up interval of the study, which may have influenced the prevalence findings of the study. Intraobserver variability may have also limited the generalizability of findings as nodules features were measured by a single radiologist. Future studies should focus on broadening the generalizability of these findings through a multicenter cohort with multiple radiologist readers.
Click to read the study in Radiology
Relevant Reading: Recommendations for the management of subsolid pulmonary nodules detected at CT: a statement from the Fleischner Society.
In-Depth [prospective cohort]: The resarchers collected data from the International Early Lung Cancer Program including 57,496 baseline CT scans with 64,677 follow-up studies at 12-month intervals. Among these studies, 2,392 (4.2%) baseline scans revealed nonsolid nodules, of which 73 studies revealed adenocarcinoma. Yearly follow-up CT scans identified new nonsolid nodules in 485 (0.7%) of 64,677 repeated screenings, 11 of which led to a diagnosis of lung adenocarcinoma. All adenocarcinomas diagnosed from nonsolid nodules were stage I, regardless of initial size or time to diagnosis. Nonsolid nodules were more likely to resolve or decrease in size with annual repeat CT scans than in baseline rounds (p < 0.0001). Participants with malignancies underwent various treatments with median time to treatment at 19 months (interquartile range 6–41 months). Progressive transitions to invasive disease, or development of solid nodule characteristics, were found in 22 cases prior to treatment with median transition time from nonsolid to part-solid at 25 months. Participants were followed for an average of six years and treatment via surgical intervention was curative for all study participants with detected disease, yielding a 100% survival rate with median follow-up since diagnosis of 78 months (interquartile range 45–122 months).
Image: PD
©2015 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.